سرطان القولون والمستقيم، الذي يشمل الأورام الخبيثة في القولون والمستقيم، يُعد ثالث أكثر أنواع السرطان انتشاراً عالمياً ويحتل المرتبة الثانية من حيث الوفيات المرتبطة بالسرطان [1]. في عام 2020، تم تشخيص أكثر من 1.9 مليون حالة جديدة حول العالم [2]، مما أدى إلى أكثر من 930.000 حالة وفاة [3]. يزداد خطر تطور الإصابة بسرطان القولون والمستقيم مع التقدم في السن، ويؤثر بشكل رئيسي على الأفراد الذين تبلغ أعمارهم 50 عاماً فأكثر.
يتم تصنيف تقدُم سرطان القولون والمستقيم إلى مراحل، تعكس كل منها مدى تطور المرض:
- المرحلة الأولى: يقتصر السرطان على الطبقات الداخلية من القولون أو المستقيم.
- المرحلة الثانية: يخترق الورم جدار القولون أو المستقيم بشكلٍ أعمق، ولكنه لا يصل إلى العقد اللمفاوية القريبة.
- المرحلة الثالثة: ينتشر السرطان إلى العقد اللمفاوية القريبة، ولكن ليس إلى مواقع بعيدة.
- المرحلة الرابعة: ينتشر السرطان إلى أعضاء بعيدة، مثل الكبد أو الرئتين.
تختلف معدلات البقاء على قيد الحياة لسرطان القولون والمستقيم بشكلٍ كبير اعتماداً على مرحلة التشخيص. وفقاً لجمعية السرطان الأمريكية [4]، فإن معدل البقاء النسبي على قيد الحياة لمدة 5 سنوات يبلغ حوالي 91٪ للمرحلة الأولى، و 85٪ للمرحلة الثانية، و 73٪ للمرحلة الثالثة، و 13٪ للمرحلة الرابعة [5].
من المُشجع أن التطورات في الأبحاث الطبية قد طرحت علاجات مبتكرة تمنح الأمل حتى لمرضى المرحلة المتقدمة من سرطان القولون والمستقيم. تعمل هذه العلاجات الناشئة، بما في ذلك العلاجات المناعية والعلاجات الموجهة، على تعزيز احتمالات البقاء على قيد الحياة وتحسين جودة الحياة. بفضل خطط العلاج المُخصَّصة والرعاية الشاملة، يُحقِّق العديد من المرضى هدأة ويعودون إلى حياة مُرضية.
بروتوكولات العلاج القياسية
يتم تصميم علاج سرطان القولون والمستقيم بناءً مرحلة السرطان، وموقع الورم، والصحة العامة للمريض [6].
التدخل الجراحي يظل هو طريقة العلاج الأساسية للمرحلة المبكرة من سرطان القولون والمستقيم. في المرحلة 1 من علاج سرطان القولون والمستقيم، قد تكفي الإجراءات مثل استئصال السليلة أو الاستئصال الموضعي. بالنسبة للأورام الأكثر تقدماً، يتم إجراء الاستئصال القطعي، مثل استئصال القولون أو استئصال المستقيم، لإزالة جزء الأمعاء المتأثر جنباً إلى جنب مع العقد اللمفاوية المجاورة. تكون الجراحة أكثر فعالية في المراحل الأولى والثالثة، حيث يكون السرطان موضعياً ولم ينتشر. في علاج سرطان القولون والمستقيم حسب المرحلة، تُؤخذ الخيارات الجراحية بعين الاعتبار بناءً على حجم الورم، وموقعه، وانتشاره.
العلاج الكيميائي يُعد مكوناً رئيسياً في علاج سرطان القولون والمستقيم، وخاصةً في المرحلة الثالثة والحالات النقيلية. في المرحلة الثالثة، أظهر العلاج الكيميائي المساعد الذي يتم إعطاؤه بعد الجراحة أنه يُقلل من خطر تكرار الإصابة بالسرطان ويُحسن معدلات البقاء على قيد الحياة بشكلٍ عام. بالنسبة لسرطان القولون والمستقيم النقيلي، يساعد العلاج الكيميائي على السيطرة على تقدُم الورم وتخفيف الأعراض، وبالتالي تعزيز جودة الحياة. يتم تخصيص خطط العلاج على أساس العوامل الفردية للمريض، مما يضمن نهجاً متوازناً بين الفعالية والقدرة على التحمل.
العلاج الإشعاعي يستخدم حِزماً عالية الطاقة لاستهداف وتدمير الخلايا السرطانية. وهو مفيد بشكلٍ خاص في حالات سرطان المستقيم. غالباً ما يتم إعطاء العلاج الإشعاعي قبل العملية لتقليص حجم الأورام، مما يجعلها أسهل في الإزالة ويُقلل من خطر تكرارها. في المراحل المتقدمة، يلعب الإشعاع دوراً تلطيفياً من خلال تخفيف الأعراض مثل الألم والانسداد.
خيارات علاج سرطان القولون والمستقيم الجديدة والمبتكرة
العلاج بالخلايا المتغصنة
يمثل العلاج بالخلايا المتغصنة Dendritic cell therapy علاجاً جديداً لسرطان القولون والمستقيم، وخاصةً للمرضى الذين يعانون من أشكال متقدمة أو مقاومة لعلاج المرض. الخلايا المتغصنة هي خلايا تُقدم المستضدات وتبدأ وتنظم الاستجابات المناعية. في العلاج بالخلايا المتغصنة لسرطان القولون، يتم حصاد هذه الخلايا من المريض، وتعريضها لمستضدات خاصة بالورم في بيئة معملية، ثم إعادة إدخالها إلى جسم المريض. تهدف هذه العملية إلى تحفيز جهاز المناعة للتعرف على الخلايا السرطانية ومهاجمتها بفعالية أكبر.
تم إثبات الأساس العلمي لهذه الطريقة عندما تم منح جائزة نوبل في علم وظائف الأعضاء أو الطب في عام 2011 إلى رالف ستاينمان لاكتشافه الخلايا المتغصنة ودورها الرئيسي في المناعة التكيفية [7]. مهد الطريق لتطوير علاجات مناعية قائمة على الخلايا المتغصنة.
استكشفت الدراسات السريرية فعالية اللقاحات القائمة على الخلايا المتغصنة في علاج سرطان القولون والمستقيم. على سبيل المثال، أشارت الأبحاث إلى أن الجمع بين العلاج بالخلايا المتغصنة والعلاج الكيميائي القياسي قد يُعزز تنشيط المناعة ويساهم في تراجع الورم لدى مرضى سرطان القولون والمستقيم. أظهرت هذه العلاجات المُركبة إمكانات في تحسين معدلات البقاء على قيد الحياة بشكلٍ عام وجودة حياة المرضى الذين يعانون من سرطان القولون والمستقيم النقيلي.
العلاج الكيميائي عالي الحرارة داخل الصفاق (HIPEC)
HIPEC هو أسلوب علاج جديد لسرطان القولون والمستقيم يجمع بين جراحة الاختزال الخلوي (CRS) مع التطبيق المباشر للعلاج الكيميائي الساخن في تجويف البطن. يُعد هذا النهج مفيداً بشكلٍ خاص للمرضى الذين يعانون من الداء السرطاني الصفاقي المنتشر الذي ينشأ من سرطان القولون والمستقيم. يتضمن الإجراء إزالة الأورام المرئية جراحياً، يليه توزيع عوامل العلاج الكيميائي الدافئة داخل تجويف الصفاق. تعمل الحرارة على تعزيز فعالية العلاج الكيميائي، مما يسمح بنفاذ أفضل للأنسجة واستهداف الخلايا السرطانية المجهرية المتبقية. أظهرت الدراسات السريرية أن CRS بالإشتراك مع HIPEC يمكن أن يُحسن معدلات البقاء على قيد الحياة بشكلٍ كبير.أفادت مراجعة جهازية أن معدل البقاء على قيد الحياة لمدة خمس سنوات يتراوح بين 19٪ و 51٪ للمرضى الذين يخضعون لهذا العلاج المشترك.
الدكتور مايكل ليب: "مستقبل جراحة السرطان المعقدة"
للحصول على فهم أعمق لـ HIPEC، نوصي بمشاهدة فيديو المقابلة هذا مع الدكتور مايكل ليب، رئيس قسم جراحة البطن والقولون والمستقيم في مستشفى أسكليبيوس بارمبيك. يشرح خطوة بخطوة عملية CRS مع HIPEC، ومعايير اختيار المرضى، وكيف يعمل هذا العلاج المُركب على تحسين النتائج بشكلٍ كبير للأفراد المصابين بالداء السرطاني الصفاقي المنتشر.
العلاج الكيميائي بالهباء الجوي المضغوط داخل الصفاق (PIPAC)
PIPAC هو علاج بديل لسرطان القولون والمستقيم. إنه تقنية طفيفة التوغل مُصممة لعلاج الداء السرطاني الصفاقي المنتشر، بما في ذلك الحالات الناجمة عن سرطان القولون والمستقيم. على عكس الطرق التقليدية، يعمل PIPAC على توصيل العلاج الكيميائي على شكل رذاذ مباشرة في تجويف الصفاق أثناء جراحة التنظير البطني، مما يضمن توزيعاً موحداً واختراقاً أعمق للأنسجة. هذه الطريقة مناسبة بشكلٍ خاص للمرضى الذين قد لا يكونون مُرشحين لإجراءات جراحية واسعة النطاق. أظهرت الدراسات أن PIPAC ممكن وآمن، حيث يتراوح متوسط البقاء على قيد الحياة بشكلٍ عام من 8 إلى 37.8 شهراً، اعتماداً على عوامل مختلفة. بالإضافة إلى ذلك، ظلت مؤشرات جودة الحياة مستقرة بين دورات PIPAC، مما يقترح قابلية التحمل.
الأشعة التداخلية
أصبحت الأشعة التداخلية (IR) جزء لا يتجزأ من إدارة سرطان القولون والمستقيم ، خاصةً للمرضى الذين يعانون من مرحلة متقدمة من المرض أو أولئك الذين ليسوا مُرشحين للجراحة التقليدية. باستخدام الإجراءات طفيفة التوغل والموجهة بالصور، يوفر IR علاجات موجهة يمكنها السيطرة بفعالية على نمو الورم مع تقليل الضرر الذي يلحق بالأنسجة السليمة المحيطة.
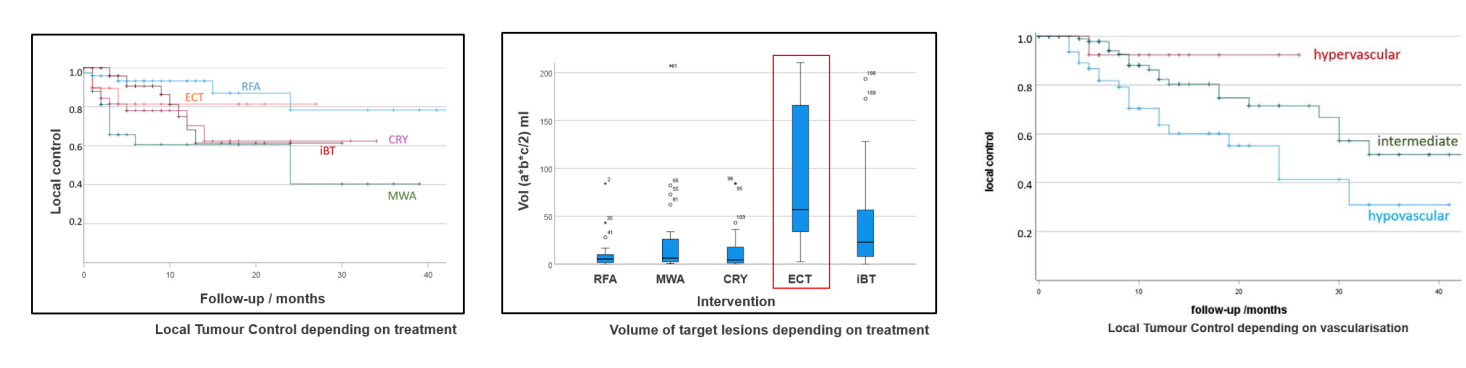
الاجتثاث الحراري يُعد أحد التقنيات IR الرئيسية، والذي يشمل الاجتثاث بالترددات الراديوية (RFA) والاجتثاث بالميكروويف (MWA). تعمل هذه الطرق على تدمير خلايا الورم عن طريق تطبيق الحرارة مباشرةً على الآفة، مما يؤدي إلى "حرق" الأنسجة السرطانية بشكل فعال مع الحفاظ على الهياكل الصحية المحيطة. أظهرت الدراسات أن الاجتثاث الحراري يمكن أن يحقق معدلات سيطرة موضعية تتراوح بين 80-90٪ ومعدلات بقاء إجمالية على قيد الحياة لمدة 5 سنوات تتجاوز 50٪ في المرضى المختارين الذين يعانون من نقائل الكبد من سرطان القولون والمستقيم. يتم تنفيذ هذه التقنيات عادةً تحت توجيه الصور (التصوير المقطعي المحوسب أو الموجات فوق الصوتية) ويمكن تكرارها إذا ظهرت آفات جديدة. تُستخدم عادةً للأورام التي تقل عن 3 سم في الحجم، وهي مثالية للمرضى غير المُرشحين للجراحة بسبب حالات صحية أخرى.
الاجتثاث بالتبريد يستخدم برودة شديدة لتحفيز موت خلايا الورم من خلال تكوين بلورات ثلجية والتمزق الخلوي. تُعتبر هذه التقنية مفيدة بشكلٍ خاص للأورام الموجودة بالقرب من الهياكل الحرجة، مثل الأوعية الدموية أو الأعصاب، لأنها توفر سيطرة دقيقة مع الحد الأدنى من الضرر للأنسجة المجاورة. كما يسمح الاجتثاث بالتبريد بالتصور في الوقت الحقيقي أثناء الإجراء، مما يُعزز الدقة. يمكن استخدامه لأغراض شافية وتلطيفية، وهو معروف بأنه يُسبب ألماً أقل بعد الإجراء مقارنةً بالاجتثاث الحراري. في بعض الحالات، يمكن أيضاً أن يؤدي إلى تحفيز استجابة مناعية ضد الورم.
البروفيسور كوفاتش يتحدث عن العلاج الكيميائي الكهربائي – كيف تساعد النبضات الكهربائية العلاج الكيميائي على أداء دوره فعلياً
العلاج الكيميائي الكهربائي (ECT) يجمع بين العلاج الكيميائي والنبضات الكهربائية لتعزيز امتصاص الخلايا السرطانية للدواء، مما يُزيد من التأثير السام للخلايا مع تقليل التعرض الجهازي. تعمل النبضات الكهربائية على زيادة نفاذية غشاء الخلية بشكلٍ مؤقت، مما يسمح للعوامل العلاجية الكيميائية باختراق الخلايا بشكل أكثر كفاءة. أظهرت الدراسات السريرية معدلات استجابة موضوعية تصل إلى 85.7٪، ومتوسط بقاء على قيد الحياة خالي من التقدُم لحوالي 9 أشهر لدى المرضى الذين يعانون من نقائل سرطان القولون والمستقيم والكبد. يُعد ECT طفيف التوغل وجيد التحمل، مما يجعله خياراً ممتازاً للمرضى الذين لديهم خيارات علاج محدودة. يتم استخدامه غالباً بالاشتراك مع علاجات أخرى ويمكن تطبيقه على الآفات الجلدية، أو الآفات تحت الجلد، أو الآفات الداخلية، بما في ذلك تلك الموجودة في منطقة الكبد أو الحوض.
تركيب دعامة هى تقنية أخرى مهمة لـ IR، وتُستخدم عادةً في المرضى المصابين بسرطان القولون والمستقيم لتخفيف انسداد الأمعاء الناجم عن نمو الورم. تحت توجيه التصوير، يتم إدخال دعامة معدنية ذاتية التوسع في الجزء الضيق من القولون أو المستقيم لاستعادة سالكية الأمعاء. يُعد هذا الإجراء مفيداً بشكلٍ خاص كجسر للجراحة، مما يمنح الوقت اللازم لاستقرار المريض قبل إزالة الورم بشكل نهائي. في الحالات المتقدمة أو غير القابلة للجراحة، يتم استخدامه كإجراء تلطيفي، لتحسين جودة الحياة من خلال تخفيف الأعراض، مثل الألم، والانتفاخ، والإمساك. يُعد تركيب الدعامة إجراءً طفيف التوغل، ولا يتطلب عادةً تخديراً عاماً، ولديه وقت تعافي سريع، مما يجعله علاجاً مناسباً لسرطان القولون للمرضى غير المُرشحين للجراحة الفورية.
الانصمام الكيميائي عبر الشرايين (TACE) هو تقنية IR تعمل على توصيل العلاج الكيميائي مباشرةً إلى أورام الكبد، مع عرقلة إمداد الدم لها في نفس الوقت. يستهدف هذا الإجراء الورم بشكل أكثر فعالية ويُقلل من التعرض الجهازي. يُعد TACE مفيداً بشكلٍ خاص لمرضى سرطان القولون والمستقيم مع نقائل الكبد، وخاصةً في المرحلتين الثالثة والرابعة، حيث قد تكون الخيارات الجراحية محدودة. في هذا الإجراء، يتم إعطاء العوامل الكيميائية العلاجية من خلال قسطرة إلى الشريان الكبدي المُغذي للورم. يتم بعد ذلك إدخال جزيئات صِمية لسد الشريان، مما يؤدي إلى حبس العلاج الكيميائي داخل الورم وحرمانه من المُغذيات. أظهر هذا النهج الموضعي نتائج واعدة. على سبيل المثال، أفادت إحدى الدراسات أن معدل السيطرة على المرض بلغ 54.3٪، ومتوسط البقاء على قيد الحياة الإجمالي بلغ 47.4 شهراً لدى المرضى الذين عولجوا بالحبيبات المُطلقة للدواء TACE.
مزايا الأشعة التداخلية
تلعب الأشعة التداخلية IR دوراً حيوياً متزايداً في المبادئ التوجيهية لعلاج سرطان القولون والمستقيم الحديثة، وخاصةً للمرضى الذين يعانون من مرض معقد أو متقدم. كبديل طفيف التوغل للجراحة التقليدية، توفر IR العديد من المزايا، بما في ذلك تقليل الرضوض الجراحية، وإقامة أقصر في المستشفى، والتعافي بشكلٍ أسرع، مما يجعلها خياراً قيماً للمرضى المعرضين لمخاطر عالية والذين لا يمكنهم الخضوع لجراحة مفتوحة. أصبحت تقنيات مثل الاجتثاث، والانصمام الكيميائي، وتركيب الدعامات جزء لا يتجزأ من مختلف أنواع علاج سرطان القولون والمستقيم، بما في ذلك التدخلات المبكرة في علاج سرطان القولون والمستقيم في المرحلة 1 والاستراتيجيات الأكثر عدوانية لـ علاج المرحلة 3 من سرطان القولون والمستقيم أو حتى علاج المرحلة الرابعة من سرطان الأمعاء. هذه الطرق موجهة للغاية، حيث تعالج الأورام مباشرةً مع الحفاظ على الأنسجة المحيطة، وهو ما يتوافق مع خوارزميات العلاج الحالية التي تهدف إلى زيادة الدقة وتقليل الآثار الجانبية الجهازية.
بالإضافة إلى ذلك، يمكن تكرار العديد من إجراءات IR، مثل الاجتثاث الحراري والعلاجات الموجهة بالتنظير البطني، بأمان، وهو أمر أساسي في إدارة المرض المتكرر أو العدواني. كما تعمل IR على توسيع نطاق تطبيقها في علاج سرطان المستقيم، والمرحلة الرابعة من سرطان المستقيم، والحالات النادرة مثل علاج سرطان الأمعاء الدقيقة أو علاج سرطان الاثنى عشر، مما يوفر خيارات مبتكرة حيث قد تفشل الطرق التقليدية. يمثل دمج IR مع العلاجات الجهازية، بما في ذلك تلك التي تتضمن الأجسام المضادة وحيدة النسيلة و العلاج المناعي لسرطان الأمعاء، تقدُماً كبيراً في طب الأورام. كجزء من فريق متعدد التخصصات، يقوم طبيب الأورام بتقييم كل حالة لتحديد متى تتناسب IR مع خطة العلاج الشاملة. من المهم أن هذه التطورات لا تُحسّن النتائج فحسب، بل تدعم أيضاً الوقاية طويلة الأمد من تكرار المرض، وإعادة تعريف معايير الرعاية عبر طيف سرطان القولون والمستقيم.
| نوع العلاج | معدل البقاء على قيد الحياة لمدة عامين | معدل الاستجابة | المدة | الآثار الجانبية |
|---|---|---|---|---|
| العلاج القياسي | ~٪25 للسرطان المتقدم | أقل من 10٪ | عدة دورات | شديدة (غثيان، وتعب، وتساقط الشعر، وكبت المناعة، وتهيُج الجلد) |
| الأساليب المبتكرة | ~٪60 للسرطان المتقدم | ٪65-45 | ما يصل إلى 4 جلسات | خفيفة (شعور موضعي بعدم الارتياح) |
* بيانات Booking Health
تكاليف الإجراءات الطبية حول العالم لسرطان القولون والمستقيم
| طريقة العلاج | ألمانيا* | بريطانيا العظمى | الولايات المتحدة الأمريكية |
|---|---|---|---|
| العلاج القياسي | 80.000 € - 150.000 € دورة كاملة | 90.000 € - 165.000 € دورة كاملة | 100.000 € - 180.000 € دورة كاملة |
| الأساليب المبتكرة | 25.000 € - 60.000 € دورة كاملة | 70.000 € - 120.000 € دورة كاملة | 100.000 € - 150.000 € دورة كاملة |
* قد تختلف الأسعار اعتماداً على دورة العلاج وخصائص الورم
قصة مريض حقيقية: النجاح مع TACE
يصبح علاج سرطان القولون والمستقيم معقداً للغاية في المراحل المتقدمة، لكن حالة ساراسيبالا بريماتشاندران من المملكة المتحدة تُظهر أن الأمل لا يزال قائماً حتى في الظروف الصعبة. بعد تشخيص إصابتها بالمرحلة الرابعة من سرطان القولون، سافرت ساراسيبالا إلى ألمانيا بمساعدة Booking Health لتلقي الرعاية من البروفيسور توماس فوجل، أحد الخبراء الرائدين في الأورام التداخلية في مستشفى جامعة غوته في فرانكفورت. خضعت لـ TACE، وهو علاج موجه وطفيف التوغل، يعمل على توصيل العلاج الكيميائي مباشرةً إلى أورام الكبد مع منع وصول الدم إليها.
سلطت ابنة ساراسيبالا، سوغاندي، الضوء على الاحترافية والتعاطف الذي لاقته طوال الرحلة العلاجية. منذ اليوم الأول، قدمت شركة Booking Health الدعم العاطفي واللوجستي المستمر، وشرحت الإجراءات، وسهلت التواصل بين الطبيب والمريض، وضمنت الوضوح في كل خطوة. سمحت هذه الرعاية للأسرة بالتركيز بشكلٍ كامل على العلاج والتعافي.
اليوم، لا يزالون متفائلين بشأن توقعات حالة ساراسيبالا. تُظهر تجربتها قوة الرعاية الشخصية والحديثة لمرضى السرطان، وكيف يمكن لأبرز مراكز الأورام وأخصائيي الأشعة التداخلية إحداث فرق. بالنسبة للمرضى الذين يواجهون علاج المرحلة الرابعة من سرطان القولون والمستقيم، فإن القصص الناجحة مثل قصة سارسيبالا تُلهم الشجاعة وتؤكد أن المساعدة الفعالة متاحة.
علاج متقدم للسرطان: قصص نجاح المرضى مع Booking Health
علاج المرحلة المتأخرة من سرطان القولون والمستقيم: نهج مُخصص
يُعد تلقي تشخيص الإصابة بسرطان القولون والمستقيم المتقدم أو في المرحلة الرابعة أمراً مُرهقاً عاطفياً. في كثير من الأحيان يُقال للمرضى "ليس هناك الكثير مما يمكن فعله،" وهو ما يمكن أن يؤدي إلى اليأس. ومع ذلك، حتى في هذه المرحلة، توجد حلول فعّالة وقوية. يستمر الطب في التطور، ومع هذا التطور، ظهرت علاجات بديلة لسرطان القولون والمستقيم يمكنها أن تُقدم الأمل وتُحسن جودة الحياة.
إن العلاجات المبتكرة، مثل TACE و HIPEC والعلاج بالخلايا المتغصنة، تعمل الآن على تغيير مشهد الرعاية للمرضى الذين يعانون من مرض نقيلي. تسمح هذه الخيارات بمجموعات علاج شخصية، مُصممة بدقة لتناسب حالة المريض وخصائص الورم. على عكس البروتوكولات التقليدية، فإن هذه الأساليب غالباً ما تؤدي إلى آثار جانبية أقل ولا تتطلب إقامة طويلة الأمد في المستشفى. هذا يجعلها قيّمة بشكلٍ خاص للأفراد الذين يسعون ليس فقط للبقاء على قيد الحياة، بل أيضاً للاستقرار والكرامة في حياتهم اليومية.
في Booking Health، نتخصص في إيصال المرضى بـ أفضل مراكز علاج سرطان القولون والمستقيم في أوروبا. باعتبارنا جهة تنسيق ودعم موثوقة، فإننا نضمن حصول المرضى على إمكانية الوصول إلى الرعاية المتقدمة القائمة على العلم. كما نُقدم أيضاً الدعم الشامل طوال الرحلة العلاجية، من التشخيص إلى العلاج، والمتابعة، والتعافي.
حتى في المراحل الأكثر تقدُماً، هناك طريق للمضي قدماً. مع الخيارات الحديثة والرعاية الاحترافية، فإن علاج المرحلة 4 من سرطان القولون والمستقيم لا يعني النهاية. بل قد يكون بدايةً لفصل جديد مليء بالأمل.
الرحلة الطبية: كل خطوة على الطريق مع Booking Health
يمكن أن يكون العثور على العلاج الأكثر فعالية لسرطان القولون والمستقيم أمراً صعباً، خاصةً بالنسبة للمرضى الذين تعبوا بالفعل من العلاجات المتعددة، والآراء المتضاربة، والمصطلحات الطبية المعقدة. مع كثرة بروتوكولات العلاج القياسية التي تُقدم نجاحاً محدوداً وغالباً ما تكون مصحوبة بآثار جانبية قاسية، غالباً ما يجد المرضى أنفسهم في حيرة من أمرهم بشأن كيفية المضي قدماً.
هذا هو المكان الذي يأتي فيه دور Booking Health. بصفتنا مُسهل طبي دولي موثوق يتمتع بخبرة تزيد عن 12 عاماً في تنسيق الأورام ، فإننا نساعد المرضى في جميع أنحاء العالم للوصول إلى العلاجات المبتكرة في أفضل المستشفيات الأوروبية. تكمُن قوتنا في بناء استراتيجيات علاج مُخصصة للسرطان، بناءً على تشخيص كل مريض، وبياناته السريرية، والتوقعات لحالته، مما يضمن ليس فقط الرعاية المتقدمة، ولكن أيضاً مساراً نحو التعافي بشكلٍ أفضل وتحسين معدلات البقاء على قيد الحياة.
توفر Booking Health تنسيق الخدمة بالكامل، بما في ذلك:
- تقييم التقرير الطبي واستشارة الخبراء
- تطوير برنامج رعاية طبية مُصمم خصيصاً
- اختيار مستشفى مناسب لعلاج سرطان القولون والمستقيم
- إعداد وترجمة الوثائق
- التواصل مع الأطباء المعالجين
- دعم التأشيرة، وترتيبات الطيران، والإقامة
- مُنسق شخصي ومترجم فوري متاحان 24/7
- الدعم قبل، وأثناء، وبعد العلاج، بما في ذلك رعاية المتابعة في بلدك الأصلي
- التسعير الشفاف بدون تكاليف خفية
صحتك مهمة جداً ولا يجب أن تتركها للصدفة. مع Booking Health، تحصل على الدعم من فريق محترف مخصص لضمان أفضل رعاية صحية متاحة، ومصممة خصيصاً لك.
الأسئلة الشائعة حول سرطان القولون والمستقيم
أرسل طلب للعلاجيتطور سرطان القولون والمستقيم في القولون أو المستقيم، وكلاهما جزءاً من الأمعاء الغليظة. يمكن أن ينشأ في أي قسم من القولون، بما في ذلك القولون الصاعد، أو المستعرض، أو النازل، أو السيني، وكذلك المستقيم.
يُعد سرطان القولون والمستقيم رابع أكثر أنواع السرطان شيوعاً في الولايات المتحدة الأمريكية، حيث يتم تشخيص حوالي 150.000 حالة جديدة سنوياً. يبلغ خطر الإصابة بهذا المرض طوال الحياة حوالي 1 من 24 بالنسبة للرجال و 1 من 26 بالنسبة للنساء.
نعم، غالباً ما يكون سرطان القولون والمستقيم قابلاً للشفاء، خاصةً عند اكتشافه في مراحله المبكرة. حتى في المرحلة الثالثة أو بعض حالات المرحلة الرابعة، يمكن لمجموعة من العلاجات المتقدمة أن تؤدي إلى هدأة طويلة الأمد وتحسُن ملحوظ في معدلات البقاء على قيد الحياة.
يتضمن التشخيص عادةً إجراء تنظير القولون مع الخزعة، ودراسات التصوير، مثل التصوير المقطعي المحوسب أو التصوير بالرنين المغناطيسي، واختبارات الدم. قد تساعد علامات الورم، مثل CEA، في تقييم استجابة العلاج ومراقبة المرض.
يُعتبر المستضد السرطاني المضغي (CEA) هو علامة الورم الأكثر استخداماً لتقييم استجابة العلاج ومراقبة تكرار سرطان القولون والمستقيم.
ينمو سرطان القولون والمستقيم ببطء على مدار عدة سنوات، ويبدأ عادةً على شكل سلائل. في حالة عدم الإزالة، قد تتحول بعض السلائل تدريجياً إلى سلائل سرطانية، لهذا السبب فإن الفحص المبكر يُعد أمراً حيوياً.
نعم، يمكن شفاء العديد من سرطانات القولون والمستقيم في المرحلة الثالثة. يشمل العلاج القياسي الجراحة متبوعة بالعلاج الكيميائي، والذي أظهر أنه يُقلل بشكلٍ كبير من خطر تكرار المرض ويحسُّن البقاء على قيد الحياة.
لا توجد إجابة واحدة تناسب الجميع، حيث يعتمد العلاج الأكثر فعالية لسرطان القولون والمستقيم على مرحلة السرطان، وموقعه، وعوامل المريض الفردية. تشمل الأساليب الشائعة الجراحة، والعلاج الكيميائي، والعلاج الموجه، والإشعاع، وفي بعض الحالات، العلاج المناعي.
خيارات العلاج لسرطان القولون والمستقيم تشمل الاستئصال الجراحي، والعلاج الكيميائي، والعلاج الإشعاعي (خاصةً لسرطان المستقيم)، والعلاجات الموجهة، والعلاج المناعي. قد تستفيد أيضاً الحالات المصابة بالمرحلة المتقدمة من التقنيات المبتكرة مثل HIPEC أو TACE.
الجراحة هي العلاج الأكثر شيوعاً، وخاصةً للمراحل الأولى والثالثة. عادةً ما يتبعها العلاج الكيميائي للقضاء على أي خلايا سرطانية متبقية وتقليل خطر تكرار المرض.
العلاج الكيميائي فعال للغاية، خاصةً في المرحلة الثالثة والمرض النقيلي. يمكنه تقليل خطر تكرار المرض بعد الجراحة، وفي الحالات المتقدمة، يُطيل العمر ويُحسّن جودة الحياة.
يُنصح بالجراحة عندما يكون السرطان موضعياً ويمكن إزالته بالكامل. عادةً ما تكون علاج الخط الأول للمرحلة المبكرة من المرض وقد تلعب أيضاً دوراً في الحالات المتقدمة المختارة ذات النقائل المحدودة.
تعتمد الآثار الجانبية على العلاج المُحدد، ولكنها قد تشمل تعب، وغثيان، وتقيؤ، وإسهال، واعتلال عصبي، وانخفاض المناعة، وتغيرات في الشهية. قد تشمل الآثار طويلة المدى خللاً في وظائف الأمعاء أو مضاعفات جراحية.
يعمل العلاج الموجه عن طريق حجب بروتينات أو مسارات معينة تعتمد عليها الخلايا السرطانية للنمو. يتم استخدامه غالباً في سرطان القولون والمستقيم المتقدم مع بعض الطفرات الجينية (على سبيل المثال RAS و BRAF و HER2)، وغالباً بالاشتراك مع العلاج الكيميائي.
يُمثل العلاج المناعي لسرطان الأمعاء باستخدام التطعيم بالخلايا المتغصنة نهجاً واعداً يعمل على تدريب جهاز المناعة على التعرّف على الخلايا السرطانية ومهاجمتها. على الرغم من أن لقاحات الخلايا المتغصنة تم تطويرها في المقام الأول لأورام الساتل الميكروي المستقرة، إلا أنها أظهرت نتائج مُشجّعة، خاصةً عند دمجها مع علاجات تقليدية.
يستخدم العلاج الإشعاعي بشكل أساسي لعلاج سرطان المستقيم، غالباً قبل الجراحة لتقليص حجم الأورام أو بعد الجراحة لتقليل تكرارها. يُستخدم بشكل أقل شيوعاً لعلاج سرطان القولون إلا إذا كان الورم ثابت أو متقدم موضعياً.
تختلف معدلات البقاء على قيد الحياة باختلاف المرحلة. يبلغ معدل البقاء النسبي على قيد الحياة لمدة خمس سنوات حوالي 91٪ للمرحلة الأولى، و 85٪ للمرحلة الثانية، و 73٪ للمرحلة الثالثة، وحوالي 13٪ للمرحلة الرابعة. يؤدي الكشف المبكر إلى تحسين النتائج بشكلٍ كبير.
نعم، التكرار ممكن، خاصةً خلال أول 3-5 سنوات بعد العلاج. تساعد المتابعة الدورية، بما في ذلك فحوصات الدم والتصوير، على اكتشاف تكرار المرض مبكراً عندما يكون أكثر قابلية للعلاج.
تختلف التكاليف بشكلٍ كبير اعتماداً على المرحلة، والموقع، وطرق العلاج، والتغطية التأمينية. في المتوسط، يمكن أن تتراوح النفقات من 25.000$ إلى أكثر من 150.000$، خاصةً إذا كانت هناك حاجة إلى علاجات متقدمة أو علاجات متعددة.
تشمل أحدث الأساليب العلاج المناعي، والعلاجات الموجهة المُركبة، والعلاجات الموضعية المبتكرة مثل HIPEC و PIPAC و TACE. توفر هذه العلاجات الأمل حتى في الحالات المتقدمة والمقاومة للعلاج سابقاً.
أفضل خيارات علاج سرطان القولون والمستقيم في عام 2025 تشمل العلاج المناعي بالخلايا المتغصنة و HIPEC و TACE. تُحقق هذه الأساليب المبتكرة معدلات استجابة تتراوح بين 45٪ و 65٪ مقارنة بأقل من 10٪ مع العلاجات القياسية، مما يوفر أملاً جديداً للحالات المتقدمة.
يعمل ممارسو الرعاية الصحية على تحسين معدلات البقاء على قيد الحياة لمرضى سرطان القولون والمستقيم المتأخر بشكلٍ كبير باستخدام العلاج الحديث من خلال تقنيات TACE و PIPAC وتقنيات الأشعة التداخلية. تُحقق هذه الأساليب طفيفة التوغل معدلات بقاء على قيد الحياة لمدة عامين تصل إلى حوالي 60٪، مقابل 25٪ باستخدام البروتوكولات التقليدية.
الفرق بين علاج سرطان القولون مقابل سرطان المستقيم يتضمن استخدام العلاج الإشعاعي. يتطلب سرطان المستقيم عادةً العلاج الإشعاعي قبل الجراحة لتقليص حجم الأورام، في حين يعتمد سرطان القولون بشكل أساسي على الجراحة والعلاج الكيميائي بدون الإشعاع الروتيني.
نعم، تشمل البدائل الاجتثاث الحراري، والاجتثاث بالتبريد، والعلاج الكيميائي الكهربائي، و TACE للمرضى غير المناسبين لإجراء جراحة. توفر هذه التقنيات طفيفة التوغل سيطرة فعالة على الورم مع فترات تعافي أقصر وآثار جانبية أقل للعلاج الموجه لسرطان القولون والمستقيم.
تُظهر تكلفة علاج سرطان القولون في أوروبا مقابل الولايات المتحدة الأمريكية اختلافات كبيرة. تُقدم ألمانيا أساليب مبتكرة بتكلفة تتراوح بين 25.000 € - 60.000 €، مقابل 100.000 € - 150.000 € في الولايات المتحدة الأمريكية. علاج سرطان القولون والمستقيم بأسعار معقولة في الخارج يوفر وفورات كبيرة مقارنةً بتكاليفه في الولايات المتحدة.
تشمل الأعراض النموذجية لسرطان القولون والمستقيم تغيرات في عادات الأمعاء، ووجود دم في البراز، وشعور بعدم الارتياح في البطن، وفقدان الوزن غير المُبرر، وتعب. مع ذلك، قد تكون المراحل المبكرة بدون أعراض، مما يؤدي غالباً إلى تأخر التشخيص.
معدل البقاء على قيد الحياة لمدة عامين لسرطان القولون والمستقيم المتقدم حوالي 25٪ باستخدام العلاجات القياسية. ومع ذلك، باستخدام الأساليب المبتكرة (مثل HIPEC أو TACE أو العلاج بالخلايا المتغصنة Dendritic cell therapy) قد ترتفع معدلات البقاء على قيد الحياة إلى حوالي 60٪، اعتماداً على تطور المرض والاستجابة للعلاج.
يتضمن علاج سرطان القولون والمستقيم القياسي عدة دورات من العلاج الكيميائي على مدى عدة أشهر. ومن ناحيةً أخرى، العلاجات المبتكرة (مثل PIPAC و HIPEC والعلاج بالخلايا المتغصنة وما إلى ذلك) تتطلب عادةً ما يصل إلى أربع جلسات.
غالباً ما تُسبب العلاجات القياسية لسرطان القولون والمستقيم غثيان، وتعب، وتساقط الشعر، وكبت المناعة. بالمقارنة، تميل العلاجات المبتكرة إلى أن تكون لها آثار جانبية أخف وموضعية، مما يُحسن التحمُل ويحافظ على جودة حياة أفضل.
عادةً ما يكون معدل الاستجابة للعلاج الكيميائي القياسي لسرطان القولون والمستقيم أقل من 10٪. في المقابل، تُحقق العلاجات المبتكرة متعددة الوسائط معدلات استجابة تتراوح بين 45-65٪، لا سيما عند الجمع بين الأساليب التداخلية، والمناعية، والموجهة.
يتطلب علاج سرطان القولون والمستقيم تحقيق توازن بين السيطرة على الورم الأولي وإدارة النقائل. في ألمانيا، يمكن للمرضى الوصول إلى العلاج بالخلايا المتغصنة و HIPEC و PIPAC والأشعة التداخلية وفرط الحرارة - تسمح هذه الأساليب بالاستهداف الدقيق للأورام (غالباً ما تُحقق نتائج تتجاوز ما يمكن أن يوفره العلاج الكيميائي القياسي).
تركز المستشفيات الرائدة في علاج سرطان القولون والمستقيم على الجمع بين الخبرة الجراحية وأحدث العلاجات. توفر مراكز الأورام الألمانية خيارات علاج متقدمة ㄧ مما يُمكن من وضع خطط علاج فردية تتكيف مع موقع الورم، ومرحلته، واستجابة المريض.
اختر العلاج في الخارج وستحصل بالتأكيد على أفضل النتائج!
المؤلفون:
تم تحرير المقال من قبل خبراء طبيين وأطباء معتمدين من مجلس الأطباء الدكتورة ناديجدا إيفانيسوفا و الدكتور بوغدان ميخالنيوك. لعلاج الحالات المشار إليها في المقال، يجب استشارة الطبيب؛ المعلومات الواردة في المقالة ليست مخصصة للتطبيب الذاتي!
سياستنا التحريرية، التي توضح بالتفصيل التزامنا بالدقة والشفافية، متاحة هنا. انقر على هذا الرابط لمراجعة سياساتنا.
المصادر:
[1] World Health Organization, WHO. سرطان القولون والمستقيم.
https://www.who.int/news-room/fact-sheets/detail/colorectal-cancer
[2] OncoDaily. سرطان القولون والمستقيم: علم الأوبئة، ومُسببات المرض، والتشخيص، والتطورات العلاجية.
https://oncodaily.com/oncolibrary/cancer-types/colorectal-cancer
[3] PubMed. العبء العالمي لسرطان القولون والمستقيم في عامي 2020 و 2040: تقديرات الإصابة والوفيات من GLOBOCAN.
https://pubmed.ncbi.nlm.nih.gov/36604116/
[4] American Cancer Society.
https://www.cancer.org/
[5] PubMed Central. علم الأوبئة لسرطان القولون والمستقيم: معدل الإصابة، والوفيات، والبقاء على قيد الحياة، وعوامل الخطر.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6791134/
[6] Cancer Research UK. خيارات العلاج لسرطان القولون.
https://www.cancerresearchuk.org/about-cancer/bowel-cancer/treatment/treatment-colon/treatment-decisions
[7] PubMed. جائزة نوبل في الطب وعلم وظائف الأعضاء لعام 2011.
https://pubmed.ncbi.nlm.nih.gov/22053831/
اقرأ:
علاجات جديدة فعالة للمرحلة الرابعة من السرطان: الابتكارات في علاج الأورام
العلاج بالخلايا المتغصنة في علاج السرطان في ألمانيا - التطعيم ضد السرطان
قائمة المقالات:
- بروتوكولات العلاج القياسية
- خيارات علاج سرطان القولون والمستقيم الجديدة والمبتكرة
- جدول العلاج المُقارن: علاجات سرطان القولون والمستقيم في الخارج
- قصة مريض حقيقية: النجاح مع TACE
- علاج المرحلة المتأخرة من سرطان القولون والمستقيم: نهج مُخصص
- الرحلة الطبية: كل خطوة على الطريق مع Booking Health
- الأسئلة الشائعة حول سرطان القولون والمستقيم
لا تعرف من أين تبدأ؟
اتصل بـ Booking Health