لا يزال سرطان البروستاتا يُشكل مصدر قلق صحي عالمي كبير، إذ يُصنف ثاني أكثر أنواع السرطان شيوعاً بين الرجال حول العالم. في عام 2022 وحده، تم الإبلاغ عن ما يقرب من 1.47 مليون حالة جديدة [1]، وهو ما يمثل 14.2٪ من جميع تشخيصات السرطان لدى الرجال [2].
فهم سرطان البروستاتا
يختلف سرطان البروستاتا في تقدُمه. بعض أنواع الأورام التي قد يصاب بها مرضى سرطان البروستاتا تكون بطيئة النمو وقد لا تتطلب علاجاً فورياً، بينما تكون أنواع سرطان البروستاتا أخرى أكثر عدوانية وتتطلب تدخلاً فورياً.
يتم تصنيف المرض عادةً إلى أربع مراحل [3]:
- المرحلة الأولى: يقتصر السرطان على البروستاتا، وعادةً ما يكون غير قابل للكشف بالفحص السريري.
- المرحلة الثانية: الورم لا يزال موجوداً داخل البروستاتا ولكن قد يكون ملموساً أثناء الاختبار المستقيمي الرقمي.
- المرحلة الثالثة: انتشر السرطان إلى أنسجة مجاورة خارج البروستاتا.
- المرحلة الرابعة: انتشر السرطان إلى أجزاء بعيدة من الجسم، مثل العقد اللمفاوية أو العظام.
قد يكون تشخيص الإصابة بسرطان البروستاتا أمراً مرهقاً. مع ذلك، من المهم أن نتذكر أن العديد من الرجال يستمرون في عيش حياة مُرضية بعد التشخيص. أدت التطورات في العلاجات الطبية، والرعاية الداعمة، وفحص سرطان البروستاتا المبكر إلى تحسين النتائج بشكل ملحوظ. مع الكشف في الوقت المناسب والعلاج الملائم، يكون هناك أساس قوي للأمل والتعافي.
علاجات سرطان البروستاتا القياسية
الإزالة الجراحية للبروستاتا، المعروفة باسم استئصال البروستاتا، تُعد علاجاً شائعاً لسرطان البروستاتا الموضعي [4]. تتضمن الجراحة المفتوحة التقليدية شقاً أكبر، في حين تستخدم التقنيات بمساعدة الروبوت robotic-assisted techniques، مثل نظام دافنشي da Vinci system، شقوقاً أصغر وتوفر دقة مُحسنة. بالمقارنة مع الجراحة المفتوحة، ارتبطت جراحة البروستاتا بمساعدة الروبوت robotic-assisted surgery بانخفاض فقدان الدم، وقصر مدة الإقامة في المستشفى، وأوقات التعافي الأسرع.
العلاج الإشعاعي يستخدم أشعة عالية الطاقة لاستهداف وتدمير الخلايا السرطانية. النوعان الرئيسيان هما العلاج الإشعاعي الخارجي (EBRT) والمعالجة الكثبية. يوجه EBRT الإشعاع من خارج الجسم، في حين تتضمن المعالجة الكثبية وضع بذور مشعة مباشرةً في البروستاتا. يمكن استخدام هذه العلاجات بمفردها أو بالاشتراك مع غيرها، وذلك اعتماداً على مرحلة وعدوانية السرطان.
العلاج الكيميائي يستخدم أدوية لقتل الخلايا السرطانية سريعة الانقسام، ويُخصص عادةً لعلاج سرطان البروستاتا المتقدم أو النقيلي. على الرغم من أن العلاج الكيميائي قد يكون له آثار جانبية، إلا أنه قد يساعد في إطالة البقاء على قيد الحياة وتخفيف الأعراض في الحالات المتقدمة.
العلاجات المبتكرة
العلاج باللوتيتيوم-177 PSMA
علاج PSMA باللوتيتيوم-177 هو علاج بالروابط المشعة مُصمم لمرضى سرطان البروستاتا النقيلي المقاوم للإخصاء (mCRPC) [5]. يجمع هذا العلاج بين نظير مشع، اللوتيتيوم-177، مع جزيء يستهدف بشكلٍ خاص مستضد غشاء البروستاتا النوعي (PSMA) الموجود على خلايا سرطان البروستاتا. عند الارتباط بالخلايا المُعبرة عن PSMA، يقوم العلاج بتوصيل الإشعاع الموجه، مما يؤدي إلى تدمير الخلايا السرطانية بشكل فعال مع تقليل الضرر الذي يلحق بالأنسجة السليمة المحيطة. أظهرت الدراسات السريرية أن نهج العلاج هذا يمكن أن يُحسّن بشكلٍ كبير معدلات البقاء على قيد الحياة ويُقلل من تقدُم المرض لدى المرضى الذين استنفدوا خيارات علاج السرطان الأخرى.
العلاج المناعي: العلاج بالخلايا المتغصنة
يمثل العلاج بالخلايا المتغصنة Dendritic cell therapy تقدماً رائداً في علاج سرطان البروستاتا، حيث يستخدم جهاز المناعة الخاص بالجسم لمكافحة الخلايا السرطانية. يتضمن هذا النهج المبتكر استخراج الخلايا المتغصنة من المريض، وتعريضها لمستضدات سرطان البروستاتا في بيئة معملية، ثم إعادة إدخالها إلى جسم المريض. الهدف هو تحفيز استجابة مناعية، مما يُمكّن الخلايا التائية T cells من التعرف على خلايا سرطان البروستاتا ومهاجمتها. تم التأكيد على أهمية الخلايا المتغصنة في العلاج المناعي عندما مُنح عالم المناعة الكندي رالف مارفن ستاينمان جائزة نوبل في علم وظائف الأعضاء أو الطب لعام 2011 لاكتشافه هذه الخلايا ودورها في المناعة التكيفية [6]. اليوم، العلاج بالخلايا المتغصنة متاح في مراكز متخصصة في جميع أنحاء العالم، بما في ذلك ألمانيا، حيث يعمل بمثابة إضافة فعالة لبروتوكولات العلاج القياسية لسرطان البروستاتا.
في المقابلة أدناه، البروفيسور فرانك جانسوج، الخبير الرائد في العلاج المناعي، يشرح دور الخلايا المتغصنة في توجيه الاستجابة المناعية للجسم ضد السرطان. كما يناقش دمج العلاج بالخلايا المتغصنة مع العلاجات التقليدية، مثل العلاج الكيميائي والعلاج الإشعاعي.
البروفيسور فرانك جانسوج يتحدث عن العلاج بالخلايا المتغصنة ودوره في علاج السرطان
العلاجات الموجهة
العلاجات الموجهة هي أدوية دقيقة مُصممة للتدخل في جزيئات أو طفرات جينية محددة تؤدي إلى نمو السرطان. في سرطان البروستاتا، تكون هذه العلاجات مفيدة بشكلٍ خاص في الحالات المتقدمة أو المقاومة للإخصاء. على سبيل المثال، تُعد مثبطات PARP فعّالة للمرضى الذين لديهم طفرات في جينات BRCA1/2 أو ATM، حيث تُعطّل آليات إصلاح الحمض النووي للخلايا السرطانية، وتؤدي إلى وفاتهم. غالباً ما تؤدي هذه العلاجات إلى آثار جانبية أقل مقارنةً بالعلاج الكيميائي التقليدي، لأنها تحافظ على الخلايا السليمة. اعتماداً على ملف السرطان المحدد للمريض، يمكن استخدام العلاجات الموجهة بمفردها أو بالاشتراك مع علاجات أخرى.
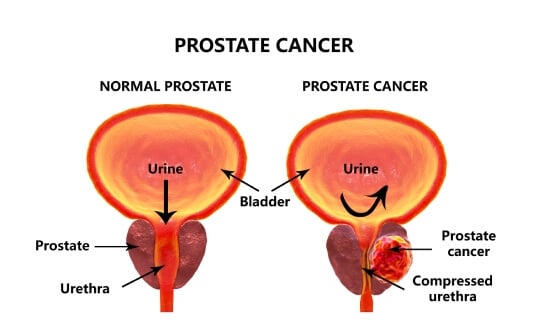
استئصال البروستاتا عبر الإحليل (TURP)
يُعد استئصال البروستاتا عبر الإحليل (TURP) إجراء جراحي يُستخدم بشكل أساسي لتخفيف أعراض المسالك البولية الناتجة عن تضخم البروستاتا، بما في ذلك الحالات التي يكون فيها التضخم ناجماً عن سرطان البروستاتا. أثناء الإجراء، يقوم الجراح بإزالة أجزاء من أنسجة البروستاتا التي تُعيق تدفق البول عبر الإحليل (مجرى البول). على الرغم من أن TURP لا يعالج سرطان البروستاتا، إلا أنه يمكنه أن يُحسن جودة الحياة بشكلٍ كبير من خلال تخفيف الأعراض مثل كثرة التبول، والإلحاح البولي، وضعف تدفق البول. يُعتبر علاجاً تلطيفياً مفيداً بشكلٍ خاص للمرضى المصابين بسرطان البروستاتا المتقدم الذين يتعرضون لانسداد المسالك البولية.
المعالجة الكثبية
المعالجة الكثبية، أو العلاج الإشعاعي الداخلي، تتضمن زرع بذور مشعة مباشرةً في غدة البروستاتا [7]. تعمل هذه الطريقة على توصيل جرعات عالية من الإشعاع إلى الورم مع تقليل التعرض للأنسجة السليمة المحيطة. هناك نوعان رئيسيان: المعالجة الكثبية بمعدل جرعة منخفض (LDR)، حيث تبقى البذور بشكلٍ دائم وتُصدر إشعاعاً على مدى عدة أشهر، والمعالجة الكثبية بمعدل جرعة مرتفع (HDR)، والتي تتضمن وضع مادة مشعة مؤقتاً لمدة قصيرة. غالباً ما يتم استخدام المعالجة الكثبية لعلاج سرطان البروستاتا الموضعي ويمكن دمجها مع العلاج الإشعاعي الخارجي للحالات الأكثر عدوانية.
العلاج الضوئي الديناميكي (PDT)
يُعتبر العلاج الضوئي الديناميكي (PDT) علاج ناشئ يستخدم أدوية حساسة للضوء يتم تنشيطها بأطوال موجية محددة من الضوء لتدمير الخلايا السرطانية. بمجرد إعطاء العامل الحساس للضوء وامتصاصه من قِبَل الخلايا السرطانية، تُعرَّض المنطقة المُستهدفة للضوء، مما يُحفِّز تفاعلاً يقضي على الخلايا الخبيثة مع الحفاظ على معظم الأنسجة السليمة. حالياً، يتوفر PDT لسرطان البروستاتا بشكل أساسي في البلدان الغربية، حيث يواصل الباحثون تقييم فعاليته وأساليب تطبيقه المُثلى. مع ذلك، تُظهر الدراسات أن طريقة العلاج هذه تُحافظ على التحكم في سلس البول ووظيفة الانتصاب لدى 100٪ و 67٪ من المرضى على التوالي.
الأشعة التداخلية (IR)
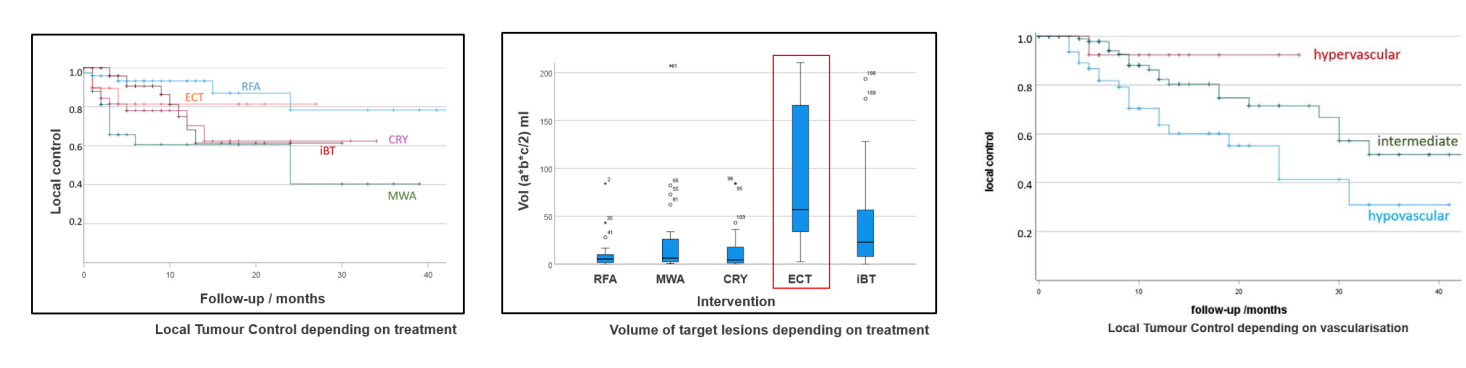
تُقدم الأشعة التداخلية (IR) علاجات طفيفة التوغل وعلاجات موجهة بالصور لسرطان البروستاتا، مما يوفر بدائل للجراحة التقليدية والعلاج الإشعاعي. تركز هذه العلاجات على استهداف الأنسجة السرطانية مع الحفاظ على الهياكل الصحية، بهدف تقليل الآثار الجانبية وتحسين أوقات التعافي.
- الاجتثاث الحراري: تقنيات الجتثاث الحراري، مثل الاجتثاث بالترددات الراديوية (RFA) والاجتثاث بالميكروويف (MWA)، تستخدم الحرارة لتدمير الخلايا السرطانية. في RFA، تُولّد التيارات الكهربائية حرارة لاجتثاث الورم، بينما تستخدم MWA الموجات الكهرومغناطيسية للغرض نفسه. تُعدّ هذه الطرق مفيدة بشكلٍ خاص لعلاج أورام البروستاتا الموضعية، ويتم توجيهها بواسطة تقنيات التصوير لضمان الدقة.
- الاجتثاث بالتبريد: يتضمن تجميد خلايا سرطان البروستاتا باستخدام مسابير التبريد cryoprobes التي يتم إدخالها إلى الورم. تؤدي البرودة الشديدة إلى تكوين بلورات ثلجية داخل الخلايا، مما يؤدي إلى موت الخلايا. تُعتبر هذه التقنية فعالة للمرضى غير المُرشحين للجراحة ويمكن استخدامها كعلاج أساسي أو بعد فشل العلاجات الأخرى. عادةً ما يتم إجراء الاجتثاث بالتبريد تحت توجيه التصوير لاستهداف الورم بدقة. تُظهر الأبحاث أن هذا العلاج يساعد في الحفاظ على التحكم في سلس البول لدى 96-100٪ من المرضى، والحفاظ على قدرة الانتصاب لدى 71-90٪ من المرضى.
- التثقيب الكهربائي غير المعكوس (IRE): هو طريقة اجتثاث غير حرارية تستخدم نبضات كهربائية لإنشاء مسام دائمة في أغشية الخلايا السرطانية، مما يؤدي إلى موت الخلايا. هذه التقنية تحافظ الأنسجة المحيطة، مثل الأعصاب والأوعية الدموية، مما يجعلها مناسبة للأورام التي تقع بالقرب من الهياكل الحرجة. يُظهر IRE نتائج واعدة كـ علاج محوري لسرطان البروستاتا، حيث يحافظ على التحكم في سلس البول لدى 100٪ من المرضى والقدرة الجنسية لدى 95٪ من المرضى.
- العلاج الكيميائي الكهربائي (ECT): يجمع بين العلاج الكيميائي مع النبضات الكهربائية لتعزيز امتصاص الدواء بواسطة الخلايا السرطانية. تعمل النبضات الكهربائية على زيادة نفاذية غشاء الخلية بشكلٍ مؤقت، مما يسمح للعوامل العلاجية الكيميائية بالدخول إلى الخلايا بشكل أكثر فعالية. في الوقت الحالي، يُعتبر تطبيق ECT في سرطان البروستاتا أمراً واعداً، حيث يُظهر نتائج إيجابية لدى مرضى سرطان البروستاتا.
- الانصمام الكيميائي عبر الشرايين (TACE): يوصل العلاج الكيميائي مباشرةً إلى ورم البروستاتا من خلال الشرايين، يليه العوامل الصِمية التي تمنع إمداد الدم، مما يحبس الدواء في الورم ويُسبب نقص التروية. أظهرت هذه الطريقة إمكانات لعلاج سرطان البروستاتا المتقدم. يُمكن تركيزات موضعية عالية للأدوية مع تقليل الآثار الجانبية الجهازية، مما يجعله مفيداً بشكل خاص للمرضى غير المُرشحين للجراحة أو العلاج الكيميائي الجهازي. يمكن أيضاً دمج TACE مع علاجات أخرى، مثل العلاج المناعي أو العلاج الإشعاعي، لتعزيز فعالية العلاج بشكلٍ عام.
البروفيسور كوفاتش: لماذا ضاعفت تقنية TACE معدل البقاء على قيد الحياة لمرضى السرطان – ما يحتاج المرضى إلى معرفته
جدول مُقارن: علاجات سرطان البروستاتا في الخارج
| نوع العلاج | معدل البقاء على قيد الحياة لمدة عامين | معدل الاستجابة | المدة | الآثار الجانبية |
|---|---|---|---|---|
| العلاج القياسي | ~٪25 للسرطان المتقدم | أقل من 10٪ | عدة دورات | شديدة (غثيان، وتعب، وتساقط الشعر، وكبت المناعة، وتهيُج الجلد) |
| الأساليب المبتكرة | ~٪60 للسرطان المتقدم | ٪65-45 | ما يصل إلى 4 جلسات | خفيفة (شعور موضعي بعدم الارتياح) |
*بيانات Booking Health
تكاليف الإجراءات الطبية حول العالم لسرطان البروستاتا
| طريقة العلاج | ألمانيا* | بريطانيا العظمى | الولايات المتحدة الأمريكية |
|---|---|---|---|
| العلاجات القياسية | 80.000 € - 150.000 € دورة كاملة | 90.000 € - 165.000 € دورة كاملة | 100.000 € - 180.000 € دورة كاملة |
| الأساليب المبتكرة | 25.000 € - 60.000 € دورة كاملة | 70.000 € - 120.000 € دورة كاملة | 100.000 € - 150.000 € دورة كاملة |
*قد تختلف الأسعار اعتماداً على مسار العلاج وخصائص الورم.
قصص واقعية: علاجات ناجحة لسرطان البروستاتا
شارك مرضى من جميع أنحاء العالم تجاربهم الإيجابية مع Booking Health، مُسلّطين الضوء على دور الشركة في تسهيل رحلاتهم العلاجية إلى الخارج.
تجربة غاري فيلوكتيت في مستشفى نورك مونشنغلادباخ
بعد تلقي تشخيص إصابته بسرطان البروستاتا، سعى غاري فيلوكتيت من الولايات المتحدة الأمريكية إلى مسار علاج يجمع بين الرعاية الطبية المتقدمة والدعم الرحيم. بعد اكتشافه لشركة Booking Health، تواصل مع فريقهم، الذي ساعده على الفور في تنسيق علاجه في مستشفى نورك مونشنغلادباخ في ألمانيا. منذ الاستشارة الأولية وحتى إتمام علاجه، شعر غاري وعائلته بدعم مستمر ومعلومات وافية. تولى فريق Booking Health جميع الجوانب اللوجستية، بما في ذلك المواعيد الطبية، وترتيبات السفر، والإقامة، مما سمح لغاري بالتركيز كلياً على تعافيه. إن احترافيتهم وتعاطفهم لم يجعل العملية أكثر كفاءة فحسب، بل قدموا أيضاً راحة نفسية خلال فترة عصيبة للغاية.
العلاج الحديث للسرطان: رحلات المرضى مع Booking Health
رحلة طبية: كل خطوة على الطريق مع Booking Health
يمكن أن يكون التنقل بين خيارات العلاج لسرطان البروستاتا المتقدم أو النقيلي أمراً مرهقاً، خاصةً بعد استنفاد العديد من العلاجات والاستشارات. إن كثرة المعلومات والبروتوكولات القياسية قد تؤدي إلى الارتباك والتعب. مع ذلك، فإن العلاجات المبتكرة المُصممة خصيصاً للحالات السريرية الفردية تُقدم الأمل في علاج البروستاتا.
تتخصص شركة Booking Health في إنشاء خطط علاج مُخصصة لسرطان البروستاتا المتقدم، بالتعاون مع مستشفيات ومتخصصين رائدين على المستوى الدولي. تشمل خدماتنا ما يلي:
- التقييم الشامل للتقارير الطبية
- تطوير برامج الرعاية الفردية
- اختيار مرافق العلاج المناسبة
- تنسيق الوثائق والاستشارات الطبية
- الدعم المستمر أثناء فترة الإقامة في المستشفى
- رعاية المتابعة بعد العلاج
- المساعدة في ترتيبات السفر والإقامة
- توفير مُنسقين ومترجمين فوريين شخصيين
- الميزانية الشفافة بدون تكاليف خفية
صحتك لا تُقدر بثمن، وإسناد إدارتها إلى مهنيين ذوي خبرة أمر بالغ الأهمية. تلتزم Booking Health بإرشادك في كل خطوة في رحلة العلاج، لضمان وصولك على علاجات مبتكرة ودعم شامل. اتصل بمستشارينا الطبيين لاستكشاف خيارات العلاج الشخصية المُصممة خصيصاً لتلبية احتياجاتك المحددة.
الأسئلة الشائعة لمرضانا حول علاج سرطان البروستاتا في الخارج
أرسل طلب للعلاجتشتهر ألمانيا بتقنياتها المتقدمة وعلاجات سرطان البروستاتا المتخصصة. كما تُقدم الولايات المتحدة الأمريكية والمملكة المتحدة رعاية صحية عالية الجودة، حيث تشتهر الولايات المتحدة الأمريكية بأبحاثها الحديثة، بينما تتميز المملكة المتحدة بنظام رعاية صحية ممتاز.
خذ في الاعتبار عوامل مثل الخبرة الطبية للبلد، وتوافر العلاجات المتقدمة، والتكلفة، والحواجز اللغوية. غالباً ما توفر ألمانيا توازناً بين الابتكار والقدرة على تحمل التكاليف.
نعم، تُقدم العديد من البلدان علاجات متقدمة، مثل الجراحة بمساعدة الروبوت Robotic-assisted surgery، والعلاج المناعي، والعلاجات الموجهة بالنويدات المشعة، مثل العلاج باللوتيتيوم-PSMA 177، والتي قد لا تكون متاحة على نطاق واسع في أماكن أخرى.
تختلف المدة: عادةً ما تتطلب الجراحة إقامة لمدة أسبوعين إلى ثلاثة أسابيع، بينما قد يمتد العلاج الإشعاعي لمدة تصل إلى شهر. سيقوم مُنسقك الطبي بتقديم جدول زمني مُصمم خصيصاً لك.
ستحتاج إلى تاريخك الطبي، وفحوصات التصوير الحديثة، وتقارير المرض، وربما فحوصات دم إضافية. قد تطلب بعض المستشفيات المزيد من التشخيصات عند الوصول.
بالتأكيد. تُقدم العديد من المستشفيات الدولية استشارات عن بُعد لتأكيد التشخيص ومناقشة خيارات العلاج قبل قيامك بالسفر.
نعم، مع التخطيط الجيد والحصول على الموافقة الطبية. حتى في ظل قيود السفر، تضمن أفضل المستشفيات في البلدان الأوروبية بيئة آمنة للمرضى الدوليين.
قد تشمل الأعراض المبكرة لسرطان البروستاتا Prostate cancer التبول المتكرر (خاصةً في الليل)، وضعف تدفق البول أو انقطاعه، وصعوبة بدء التبول، ووجود دم في البول أو السائل المنوي، والشعور بعدم الارتياح في منطقة الحوض. تكون العديد من الحالات بدون أعراض في المراحل المبكرة، مما يجعل الفحص أمراً مهماً.
تختلف تكلفة علاج سرطان البروستاتا في ألمانيا باختلاف الطريقة والمستشفى. تتراوح تكلفة العلاج باستخدام الطرق القياسية عادةً من 80.000 € إلى 150.000 € للدورة الكاملة، في حين أن الإجراءات المبتكرة قد تكلف ما بين 25.000 € و 60.000 €.
يشمل أحدث علاج لسرطان البروستاتا في ألمانيا العلاج بالنويدات المشعة باللوتيتيوم-177 PSMA، والعلاج الهرموني المتقدم، والجراحة بمساعدة الروبوت Robotic-assisted surgery (دافنشي Da Vinci) وتقنيات الإشعاع الدقيقة. تُحسّن هذه الخيارات النتائج وتُقلل من الآثار الجانبية.
نعم، العلاج المناعي لسرطان البروستاتا – بما في ذلك العلاج بالخلايا المتغصنة Dendritic cell therapy ومثبطات نقاط التفتيش المناعية – يتم استخدامه في الحالات المتقدمة أو المتكررة. قد يُعزز ذلك قدرة جهاز المناعة على مكافحة السرطان وغالباً ما يتم دمجه مع العلاجات التقليدية.
نعم، تشمل العلاجات غير الجراحية لسرطان البروستاتا المراقبة النشطة، والعلاج الإشعاعي، والعلاج الهرموني، والمعالجة الكثبية، والعلاج المناعي. هذه الخيارات مناسبة للمرضى في المرحلة المبكرة أو أولئك غير المؤهلين للجراحة.
معدل نجاح علاج سرطان البروستاتا في ألمانيا مرتفع، حيث يتجاوز البقاء على قيد الحياة لمدة 5 سنوات 90٪ في حالة المرض الموضعي. يعتمد النجاح على المرحلة، والعلاج المُختار، والصحة العامة للمريض، لكن النتائج من بين الأفضل في أوروبا.
نعم، لا يتطلب علاج سرطان البروستاتا في ألمانيا بالنسبة للمرضى الدوليين إحالة محلية. يُقدم مُنسقو السفر الطبي المساعدة في إعداد الوثائق، وجدولة المواعيد، والترجمة الفورية، ودعم التأشيرة لتبسيط العملية.
قد تشمل تغييرات نمط الحياة أثناء علاج سرطان البروستاتا اتباع نظام غذائي غني بالنباتات، وتقليل الدهون المُشبعة، وممارسة الرياضة بانتظام، وإدارة التوتر، والإقلاع عن التدخين، والحد من تناول الكحول – كلها أمور تدعم التعافي والصحة على المدى الطويل.
بالنسبة للمرحلة الرابعة من سرطان البروستاتا أو سرطان البروستاتا المتقدم، فإن معدل البقاء على قيد الحياة لمدة عامين مع الخيارات العلاجية القياسية (مثل العلاج الهرموني، أو العلاج الكيميائي، أو العلاج الإشعاعي) يبلغ حوالي 25٪. في المقابل، مع العلاجات المبتكرة (مثل علاج PSMA باللوتيتيوم-177 أو العلاج المناعي بالخلايا المتغصنة أو الانصمام الكيميائي عبر الشرايين (TACE) أو الاجتثاث)، يمكن أن يصل معدل البقاء على قيد الحياة إلى حوالي 60٪.
ما هي معدلات الاستجابة النموذجية لسرطان البروستاتا المتقدم باستخدام العلاجات القياسية مقابل العلاجات المبتكرة؟
في سرطان البروستاتا المتقدم، غالباً ما يُحقق العلاج الجهازي القياسي معدل استجابة أقل من 10٪. ومع ذلك، فإن العلاجات المبتكرة (مثل العلاج بالنوديات المشعة الموجه لـ PSMA أو العلاج بالخلايا المتغصنة أو TACE أو الاجتثاث الموضعي) قد توفر معدلات استجابة تتراوح بين 45-65٪.
بالنسبة لسرطان البروستاتا المتقدم، تتضمن العلاجات القياسية عادةً دورات متعددة من العلاج الكيميائي أو العلاج الهرموني على مدى عدة أشهر. في المقابل، فالأساليب المبتكرة (مثل TACE أو الاجتثاث بالتبريد أو العلاج بالخلايا المتغصنة) عادةً ما يتم إستكمالها في ما يصل إلى أربع جلسات.
ما هي الآثار الجانبية الشائعة أثناء علاج سرطان البروستاتا المتقدم، وكيف تختلف بين الأساليب القياسية والأساليب المبتكرة؟
يمكن أن تُسبب علاجات سرطان البروستاتا القياسية آثار جانبية كبيرة مثل التعب، والغثيان، وتساقط الشعر، وكبت المناعة. أما الخيارات العلاجية المبتكرة (مثل علاج PSMA باللوتيتيوم-177 أو العلاج المناعي بالخلايا المتغصنة أو الاجتثاث الحراري) تميل إلى التَسبُب في آثار موضعية خفيفة فقط مثل شعور موضعي بعدم الارتياح أو حُمى منخفضة الدرجة.
يعتمد علاج سرطان البروستاتا على المرحلة، وخصائص الورم، والحالة الصحية العامة للمريض. تشمل الخيارات العلاج باللوتيتيوم-177 والعلاج بالخلايا المتغصنة، والعلاج الموجه، والمعالجة الكثبية، والعلاج الضوئي الديناميكي، والأشعة التداخلية (للسيطرة الموضعية أو إدارة الأعراض).
اختر العلاج في الخارج وستحصل بالتأكيد على أفضل النتائج!
المؤلفون:
تم تحرير المقال من قبل خبراء طبيين وأطباء معتمدين من مجلس الأطباء الدكتورة ناديجدا إيفانيسوفا و الدكتور بوغدان ميخالنيوك. لعلاج الحالات المشار إليها في المقال، يجب استشارة الطبيب؛ المعلومات الواردة في المقالة ليست مخصصة للتطبيب الذاتي!
سياستنا التحريرية، التي توضح بالتفصيل التزامنا بالدقة والشفافية، متاحة هنا. انقر على هذا الرابط لمراجعة سياساتنا.
المصادر:
[1] Research Gate. التباين الدولي في معدلات الإصابة والوفيات بسرطان البروستاتا.
https://www.researchgate.net/publication/221713090_International_Variation_in_Prostate_Cancer_Incidence_and_Mortality_Rates
[2] Pharmaceuticals. إحداث ثورة في الكشف عن سرطان البروستاتا: دور عوامل التصوير المعتمدة.
https://www.mdpi.com/1424-8247/18/6/906
[3] American Cancer Society. مراحل سرطان البروستاتا.
https://www.cancer.org/cancer/types/prostate-cancer/detection-diagnosis-staging/staging.html
[4] Prostate Cancer UK. الجراحة: استئصال البروستاتا الجذري.
https://prostatecanceruk.org/prostate-information-and-support/treatments/surgery
[5] The New England Journal of Medicine. اللوتيتيوم Lutetium-177–PSMA-617 لسرطان البروستاتا النقيلي المقاوم للإخصاء.
https://www.nejm.org/doi/full/10.1056/NEJMoa2107322
[6] PubMed. جائزة نوبل في في علم وظائف الأعضاء أو الطب لعام 2011.
https://pubmed.ncbi.nlm.nih.gov/22053831/
[7] Cancer Research UK. المعالجة الكثبية لسرطان البروستاتا.
https://www.cancerresearchuk.org/about-cancer/prostate-cancer/treatment/radiotherapy/brachytherapy
اقرأ:
قائمة المقالات:
لا تعرف من أين تبدأ؟
اتصل بـ Booking Health