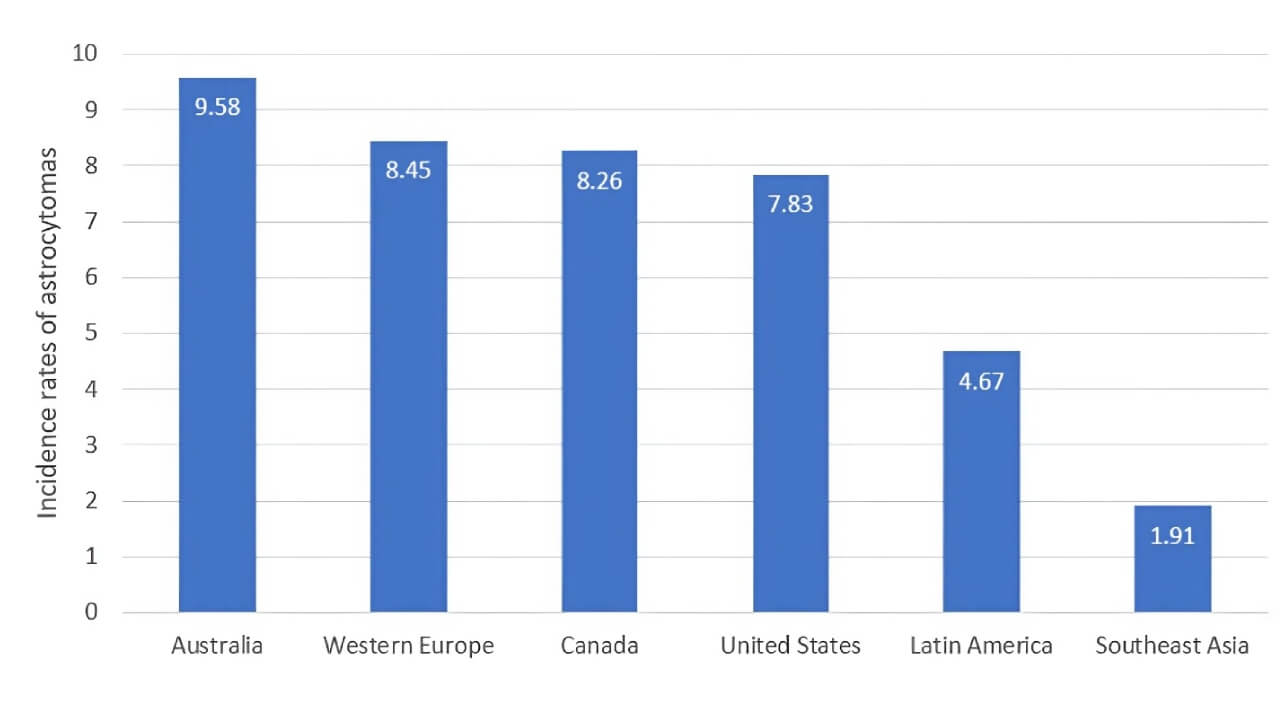
الورم النجمي Astrocytoma هو نوع من الأورام الدبقية ينشأ من الخلايا النجمية على شكل نجمة في الدماغ، ويتراوح من الشكل بطيء النمو نسبياً (الدرجات I–III) إلى الشكل شديد العدوانية من الدرجة الرابعة، الورم الأرومي الدبقي Glioblastoma. في الولايات المتحدة، تحدث الأورام الدبقية Gliomas بمعدل حوالي 6 حالات لكل 100.000 شخص سنوياً، حيث يمثل الورم الأرومي الدبقي حوالي 61٪ من هذه الحالات وتمثل الأورام النجمية غير الأرومية الدبقية حوالي 19٪ [1]. كل عام، يتم تشخيص ما يقرب من 25.400 ورم خبيث في الدماغ أو النخاع الشوكي (خاصة الورم النجمي الشوكي)، مما يؤدي إلى حوالي 18.760 حالة وفاة. الورم الأرومي الدبقي، وهو النوع الأكثر فتكاً، يصيب حوالي 3.2 حالة لكل 100.000 شخص سنوياً، ويبلغ متوسط عُمر التشخيص ~64 عاماً.
سريرياً، التمييز بين الورم النجمي مقابل الورم الأرومي الدبقي مهم وواضح. فبينما يتميز الورم الأرومي الدبقي بالتطور السريع وضعف معدلات البقاء على قيد الحياة، فإن الأورام النجمية منخفضة الدرجة، بما في ذلك الورم النجمي من الدرجة الثانية، غالباً ما يكون لها مسار أبطأ ولكنها لا تزال تتطلب مراقبة دقيقة بسبب خطر التحول إلى أشكال أكثر عدوانية مع مرور الوقت.
هذه التوقعات المتشائمة تؤكد على الحاجة المُلحة إلى علاج جديد وأكثر فعالية لعلاج الورم النجمي في الدماغ.
طرق العلاج القياسية: الجراحة، والعلاج بالبروتونات، والإشعاع
في الممارسة السريرية الحالية، علاج الورم النجمي في الدماغ يتضمن عادةً مزيجاً من الجراحة والاستراتيجيات القائمة على الإشعاع. تهدف هذه الوسائل العلاجية الراسخة إلى تخفيف عبء الورم وتأخير تقدمه، على الرغم من اختلافها في الدقة، والآثار الجانبية، والنتائج طويلة الأمد.
تقنيات جراحة الأعصاب المتقدمة في إدارة الورم النجمي
جراحة الدماغ الحديثة لم تعد تُعرف بالشقوق الكبيرة والمخاطر العصبية العالية. بفضل التقدم التكنولوجي، تُقدم تقنيات جراحة الأعصاب اليوم تدخلات أكثر استهدافاً وأكثر أماناً - حتى للأورام التي كانت تُعتبر سابقاً غير قابلة للجراحة. فيما يلي أهم الابتكارات الرئيسية التي تُحدد الآن جراحة الورم النجمي الحديثة.
جراحة التنظير الداخلي عن طريق الأنف (EES)
هذا النهج الجراحي طفيف التوغل يصل إلى الورم عبر الممرات الأنفية، مما يلغي الحاجة إلى جراحة حج القحف (فتح الجمجمة). إنه فعال بشكل خاص في حالات الأورام النجمية في الخط الناصف أو قاعدة الجمجمة. بتجنُب سحب أنسجة الدماغ، يُقلل EES بشكل كبير من وقت التعافي، ومضاعفات ما بعد الجراحة، والندوب المرئية. غالباً ما يُبلغ المرضى عن عودة أسرع إلى الوظائف الطبيعية، خاصةً عندما يكون الورم بالقرب من العصب البصري أو منطقة الغدة النخامية.
حج القحف بتقنية ثقب المفتاح Keyhole
تستخدم تقنيات ثقب المفتاح Keyhole فتحات أصغر موضوعة بشكل استراتيجي للوصول إلى الأورام مع الحد الأدنى من الاضطراب لهياكل الدماغ الصحية. يسمح هذا النهج بإزالة الورم بدقة مع الحفاظ على الوظائف العصبية الحيوية. أظهرت النتائج السريرية انخفاض فقدان الدم، وقصر مدة الإقامة في المستشفى، وانخفاض خطر العدوى مقارنةً بجراحة حج القحف التقليدية المفتوحة.
تخطيط الدماغ أثناء اليقظة
بالنسبة للأورام القريبة من مناطق اللغة أو الحركة، يُساعد حج القحف أثناء اليقظة مع التخطيط أثناء الجراحة على تحديد وظائف الدماغ الحيوية والحفاظ عليها أثناء الاستئصال. يتم تخدير المرضى تخديراً خفيفاً لكنهم في حالة وعي كافية لأداء مهام، مما يسمح للجراحين بتجنب مناطق القشرة الدماغية البليغة بدقة. أدت هذه التقنية إلى تحسين جودة الحياة بشكل كبير وتعتبر الآن المعيار الذهبي للجراحة في مناطق الدماغ الوظيفية.
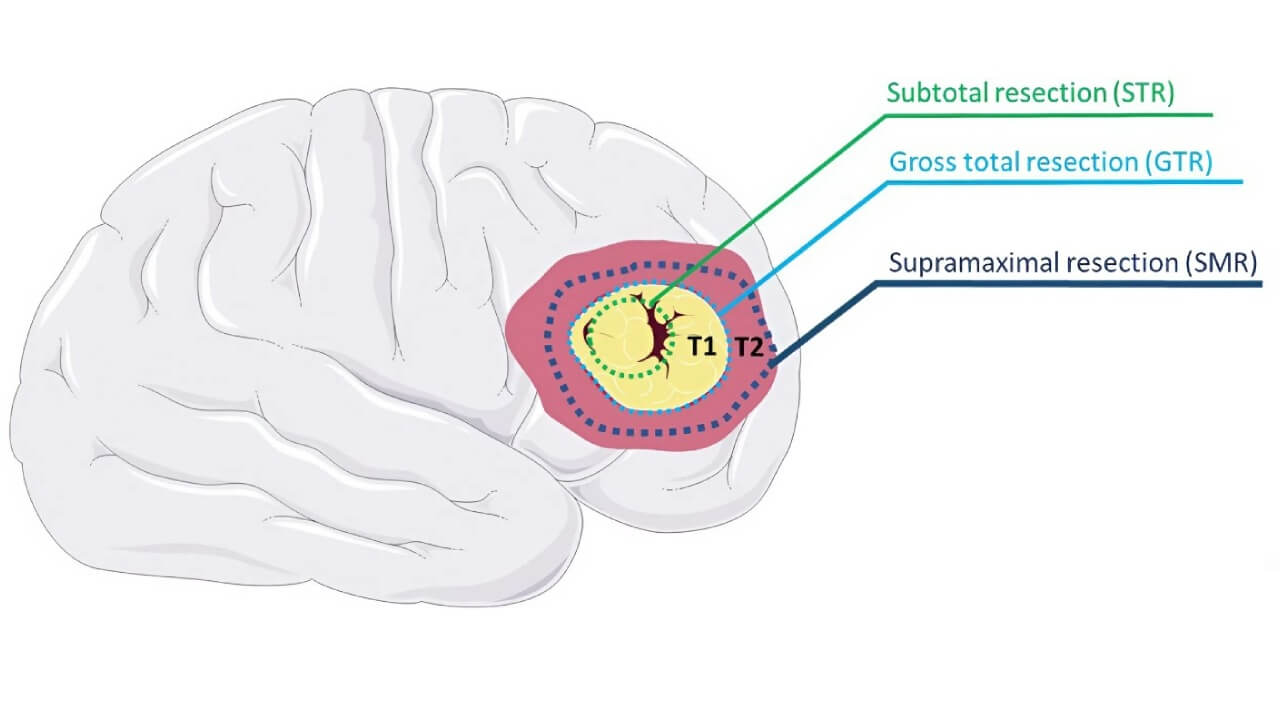
يُلخص الرسم التوضيحي أدناه الاستراتيجيات الجراحية الحالية، مُطابقةً لموقع الورم ودرجته. تُوسّع هذه الخيارات نطاق العلاج للمرضى الذين يعانون من كل من الأورام النجمية منخفضة الدرجة وعالية الدرجة.
العلاج بالبروتونات
العلاج بحزم البروتونات (العلاج بالبروتون) Proton Therapy يقوم بتوصيل الإشعاع باستخدام جسيمات مشحونة إيجابياً تُطلق معظم طاقتها مباشرةً في موقع الورم - ظاهرة تُعرف باسم ذروة براغ. يسمح هذا بانخفاض حاد في الإشعاع بعد الهدف، مما يُقلل من التعرض لهياكل الدماغ السليمة المحيطة ويقضي عملياً على "جرعة الخروج". انحدار الجرعة التدريجي هذا يجعل العلاج متوافقاً للغاية، مما يُمكّن من استهداف الورم بدقة مع تجنب المناطق الوظيفية المجاورة. وجدت مراجعة منهجية شملت أكثر من 800 مريض مصاب بالورم الدبقي (الدرجات II–IV) معدلات بقاء على قيد الحياة قابلة للمقارنة بالعلاج الإشعاعي التقليدي، مع مزايا ملحوظة في الحفاظ على المناطق الإدراكية والعصبية الحساسة [3]. كشفت مقارنات قياس جرعات الإشعاع مع VMAT و 3D-CRT عن انخفاض في متوسط الجرعة يصل إلى 99٪ في حُصَين الجانب المقابل - مما يُسلط الضوء على إمكاناته في الحفاظ على الوظيفة العصبية الإدراكية [4].
العلاج الإشعاعي الدقيق
يُعد العلاج الإشعاعي مُكوناً أساسياً في علاجات الورم النجمي، خاصةً بعد الاستئصال الجراحي. فهو يستهدف خلايا الورم المتبقية التي لا يمكن إزالتها بأمان ويساعد على تأخير تقدُم المرض. تتضمن البروتوكولات القياسية عادةً جلسات يومية على مدى فترة ستة أسابيع، مُوصِلةً جرعة إجمالية تبلغ حوالي 50-60 جراي.
عند إعطائه في نظام علاجي متعدد الوسائط، ثبت أن الإشعاع يُحسّن النتائج بشكل كبير. أفادت إحدى التجارب السريرية الكبيرة بتضاعف معدل البقاء على قيد الحياة لمدة عامين عندما تم الجمع بين الإشعاع والعلاج الجهازي، مقارنة بالإشعاع وحده [5].
طرق التوصيل المتقدمة مثل العلاج الإشعاعي ذو الشدّة المعدّلة (IMRT) والعلاج بالقوس الحجمي المعدّل (VMAT) تسمح للأطباء بتشكيل جرعة الإشعاع لتتوافق بدقة مع البنية ثلاثية الأبعاد للورم. هذا يُقلل من التعرض الجانبي لمناطق الدماغ الحرجة، مما يُقلل من خطر التدهور المعرفي والآثار الجانبية الأخرى.
إعادة برمجة المناعة: كيف يُسهم العلاج بالخلايا المتغصنة في تشكيل مستقبل رعاية أورام الدماغ
من خلال تسخير دفاعات الجسم المناعية، يبرُز العلاج بالخلايا المتغصنة Dendritic cell therapy كعلاج تحويلي لعلاج الورم النجمي. وباعتباره شكلاً مُخصصاً للغاية من أشكال العلاج المناعي، فإنه يُعلّم الجهاز المناعي التعرف على خلايا الورم والقضاء عليها بشكل انتقائي - مما يوفر نهج دقيق الاستهداف مع آثار جانبية جهازية أقل من العلاجات التقليدية.
كيف يعمل
تلعب الخلايا المتغصنة Dendritic cells دوراً محورياً في الاستجابة المناعية من خلال تقديم المستضدات للخلايا التائية T-cells، حيث "تُعلّم" جهاز المناعة بشكل أساسي ما يجب مهاجمته. تم اكتشاف هذه الآلية المهمة من قِبل عالم المناعة الكندي رالف م. ستاينمان، الحائز على جائزة نوبل في الطب أو علم وظائف الأعضاء لعام 2011 لاكتشافه [6].
في الاستخدام السريري، يتضمن العلاج بالخلايا المتغصنة Dendritic cell therapy جمع الخلايا المناعية الخاصة بالمريض، وتحميلها بمستضدات الورم في المختبر، ثم إعادة إدخالها إلى الجسم. بمجرد تنشيطها، تستطيع هذه الخلايا المتغصنة اختراق الحاجز الدموي الدماغي وتوجيه الجهاز المناعي لاستهداف خلايا الورم النجمي بدقة عالية.
لماذا هذا مهم في علاج الورم النجمي
على عكس العلاج الإشعاعي والعلاج الكيميائي التقليدي، اللذان يؤثران على الأنسجة السليمة والسرطانية على حدٍ سواء، يركز العلاج بالخلايا المتغصنة الاستجابة المناعية حصرياً على الخلايا الخبيثة. تُعد هذه الخاصية بالغة الأهمية في علاج البنى الدقيقة الحساسة مثل الدماغ.
تشمل الفوائد الرئيسية ما يلي:
- الاستهداف الانتقائي: تأثير مُركّز ضد خلايا الورم النجمي مع الحفاظ على أنسجة الدماغ السليمة.
- تنشيط المناعة التكيفية: يمكن أن تتطور الاستجابة المناعية مع تحور الورم، مما يقلل من خطر الانتكاس.
- حماية مُطوّلة: تُمكّن الذاكرة المناعية من المراقبة المُستمرة ضد نمو الخلايا السرطانية مُجدداً.
- سُمية أقل: يُبلغ المرضى عن آثار سلبية أقل مُقارنةً بالعلاجات القياسية عالية الجرعة.
- الوصول إلى الحاجز الدموي الدماغي: الخلايا المتغصنة (الخلايا الشجيرية) قادرة على الوصول إلى مواقع ورم الدماغ التي لا تستطيع العديد من الأدوية الوصول إليها.
إذا كنت تبحث عن خيارات علاج الورم النجمي، وخاصة في الحالات التي أظهرت فيها الطرق التقليدية فائدة محدودة، فقد يوفر لك هذا العلاج المناعي المبتكر للورم النجمي أملاً جديداً.
الأدلة السريرية وحالات الاستخدام
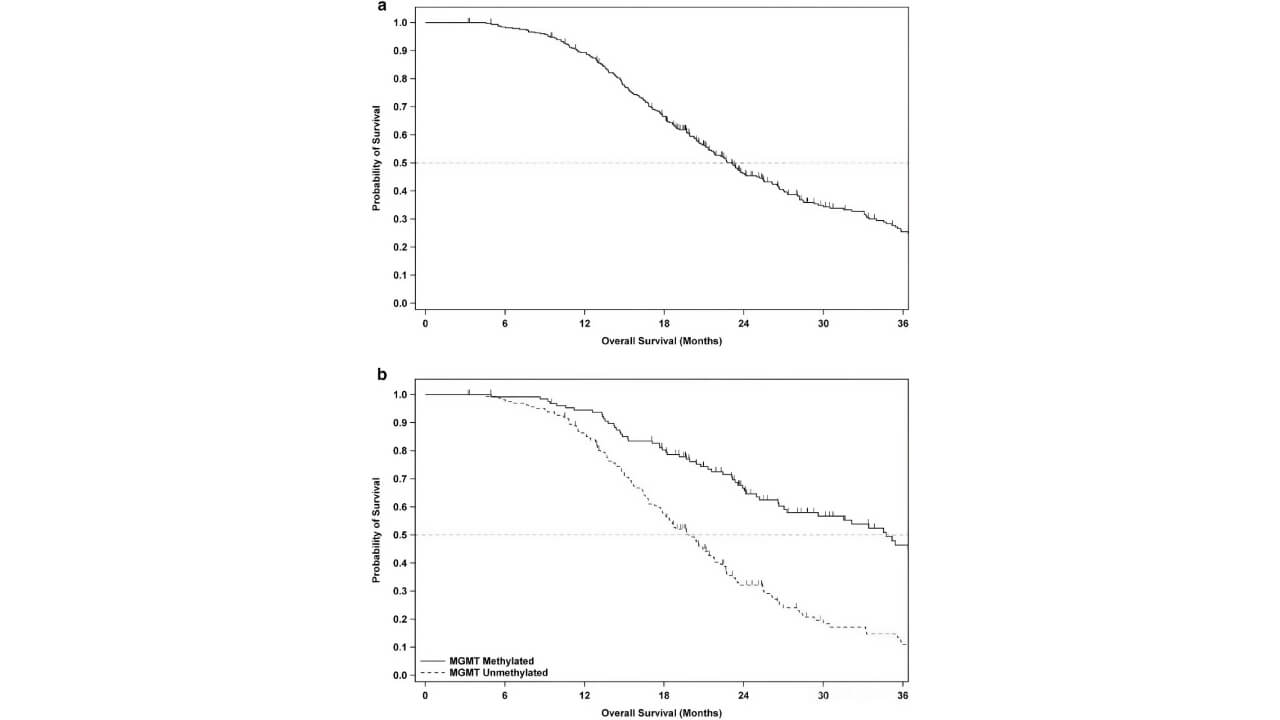
أظهرت دراسات حديثة في المرحلة الثالثة نتائج مشجعة. إحدى التجارب واسعة النطاق شملت أكثر من 300 مريض بالورم الأرومي الدبقي وجدت أن إضافة لقاح الخلايا المتغصنة إلى الرعاية القياسية أدى إلى زيادة متوسط البقاء على قيد الحياة الإجمالي وحسّن بشكل ملحوظ معدلات البقاء على قيد الحياة لمدة خمس سنوات - من 5.7٪ إلى أكثر من 13٪ [7]. وكانت الآثار الجانبية ضئيلة جداً واقتصرت في الغالب على أعراض خفيفة تشبه أعراض الإنفلونزا.
يتم حالياً النظر في هذا النهج عبر مراحل الورم النجمي المختلفة، بما في ذلك:
- بعد الاستئصال الجراحي، لاستهداف خلايا الورم المتبقية.
- كجزء من أنظمة علاجية متعددة الوسائط، تُكمّل العلاج الإشعاعي والعلاجات الجهازية الأخرى.
- في حالات أورام الدماغ النجمية المتكررة أو غير القابلة للجراحة، حيث قد تكون الخيارات الأخرى محدودة.
إنه ذو قيمة خاصة للمرضى الذين يبحثون عن علاجات جديدة للورم الدبقي تتجاوز الأساليب التقليدية.
علاجات جديدة للورم النجمي في الدماغ: تقنيات الأشعة التداخلية
بالنسبة للمرضى الذين يعانون من أورام نجمية تقع في مناطق خطرة من الناحية الجراحية، فإن الإجراءات طفيفة التوغل الموجهة بالتصوير تقدم بديلاً آمناً وفعالاً. أصبحت الأشعة التداخلية جزءاً أساسياً من أدوات طب الأورام العصبية الحديث - خاصةً عندما تكون الأورام عميقة، أو قريبة من مراكز الدماغ الحيوية، أو متكررة بعد العلاج القياسي. تُساعد هذه الأساليب المتقدمة على تقليل المضاعفات الجراحية، وتعزيز السيطرة على الورم موضعياً، وقد تُحسّن النتائج عند دمجها مع العلاجات الجهازية.
العلاج الحراري الخلالي بالليزر (LITT)
يستخدم العلاج الحراري الخلالي بالليزر LITT طاقة الليزر المركزة لاجتثاث أنسجة الورم من الداخل، بتوجيه في الوقت الفعلي بواسطة التصوير بالرنين المغناطيسي MRI. تقدم هذه الطريقة العديد من الفوائد السريرية المهمة:
- الوصول إلى الورم من خلال فتحة صغيرة في الجمجمة مع الحد الأدنى من الاضطراب للأنسجة المحيطة
- تستخدم التصوير بالرنين المغناطيسي في الوقت الفعلي لتوجيه توصيل الحرارة، مما يضمن تحكماً دقيقاً في الضرر الحراري
- تحافظ على هياكل الدماغ الصحية بينما تُدمر خلايا الورم بفعالية
- مناسِبة بشكل خاص للأورام الصغيرة والمرضى الذين لا يستطيعون الخضوع للجراحة التقليدية
- قد تفتح الحاجز الدموي الدماغي مؤقتاً، مما يُحسّن توصيل العلاجات اللاحقة
أظهر هذا النهج نتائج بقاء على قيد الحياة إيجابية لدى مرضى مُختارين يعانون من أورام دبقيه عميقة أو متكررة.
العلاج الكيميائي الكهربائي
يُعزز العلاج الكيميائي الكهربائي Electrochemotherapy امتصاص الدواء في الخلايا السرطانية باستخدام نبضات كهربائية تزيد نفاذية الغشاء مؤقتاً. تُقدم هذه الاستراتيجية المُستهدِفة العديد من المزايا الرئيسية:
- تُوصل نبضات كهربائية عبر أقطاب كهربائية دقيقة تُوضع عبر فتحة صغيرة في الجمجمة
- تسمح لعوامل العلاج الكيميائي بدخول خلايا الورم بكفاءة أكبر بكثير - امتصاص أعلى يصل إلى 300 مرة
- يقتصر تأثيرها على المنطقة المعالجة فقط، مع تجنُب أنسجة الدماغ السليمة
- يمكن إجراؤها في جلسة واحدة، بما في ذلك أثناء العملية الجراحية عندما يكون ذلك مناسباً
تُعد هذه التقنية واعدة بشكل خاص للأورام في المناطق البليغة أو المعقدة جراحياً.
الانصمام
يُستخدم الانصمام Embolization لحجب تدفق الدم إلى الورم قبل الجراحة، مما يقلل النزيف أثناء العملية ويحسّن نتائج الاستئصال. تقدم هذه الخطوة التحضيرية فوائد متعددة:
- تُحدد وترسم خرائط الشرايين المغذية للورم عبر تصوير الأوعية الدموية
- توصل المواد الانصمامية (الجسيمات، أو المواد اللاصقة، أو اللفائف) عبر قسطرة دقيقة
- تقلل النزيف أثناء الجراحة، مما يسمح بإزالة الورم بشكل أكثر اكتمالاً وأكثر أماناً
- يتم إجراؤها قبل 24-48 ساعة من الاستئصال لضمان أقصى قدر من الفعالية
- مفيدة بشكل خاص في حالات الأورام النجمية التي تحتوي على كثافة عالية من الأوعية الدموية أو الآفات القريبة من هياكل الدماغ الحرجة
هذه التقنية راسخة في التخطيط الجراحي العصبي وتستمر في التطور مع عوامل الانصمام (عوامل الانسداد) الأحدث والتوجيه التصويري.
| نهج العلاج | معدل الاستجابة | فائدة البقاء على قيد الحياة | الآثار الجانبية | مدة العلاج | نطاق تكلفة العلاج (أوروبا) |
|---|---|---|---|---|---|
| الجراحة | 60 - ٪80 (المراحل المبكرة من الورم الأرومي الدبقي) 20 - ٪30 (المراحل المتقدمة) | الأساس للعلاجات الأخرى | الألم، وخطر العدوى، ووقت التعافي | إجراء لمرة واحدة | 25.000 € - 50.000 € |
| الإشعاع التقليدي | 40 - ٪60 (المراحل المبكرة) 15 - ٪20 (المراحل المتقدمة) | جزء من البروتوكول القياسي | التعب، وتهيج الجلد، والتأثيرات المعرفية | 6 أسابيع (جلسات يومية) | 28.000 € - 42.000 € |
| العلاج بالبروتونات | 50 - ٪70 (المراحل المبكرة) 15 - ٪25 (المراحل المتقدمة) | مشابه للإشعاع التقليدي مع آثار جانبية أقل | خفيفة إلى معتدلة | 6 أسابيع (جلسات يومية) | 56.900 € - 90.500 € |
| العلاج بالخلايا المتغصنة | 85 - ٪95 (المراحل المبكرة) 60 - ٪80 (المراحل المتقدمة) | إمكانية تحقيق فائدة البقاء على قيد الحياة طويل الأمد | الحد الأدنى (أعراض تشبه أعراض الأنفلونزا في المقام الأول) | إجراء لمرة واحدة مع تأثيرات دائمة | 20.000 € - 38.000 € |
| العلاج الكيميائي الكهربائي | ~٪70 استجابة كاملة في الدراسات | تحسن متوسط البقاء على قيد الحياة لمدة 9-14 شهراً | تأثيرات موضعية، تأثير جهازي ضئيل جداً | جلسة واحدة | 30.000 € - 45.000 € لكل دورة علاجية |
| العلاج الحراري الخلالي بالليزر | أفضل للأورام التي يقل حجمها عن 11 سم مكعب | ~11.5 شهراً للمرض المتكرر | الحد الأدنى | إجراء لمرة واحدة | جزء من التكاليف الجراحية |
من التشخيص إلى التعافي
عندما بدأ ماركو، مهندس معماري يبلغ من العمر 42 عاماً من شمال إيطاليا، يعاني من فقدان الذاكرة قصيرة الأمد ونوبات من الارتباك، لم يُعر الأمر اهتماماً كبيراً. ولكن في غضون أسابيع، تطورت الأعراض إلى اضطرابات بصرية وتردُد في الكلام. أكد تصوير الدماغ بالرنين المغناطيسي السبب: ورم نجمي منخفض الدرجة يؤثر على الفص الصدغي الأيسر.
عرض الأطباء في إيطاليا الاستئصال القياسي والعلاج الإشعاعي، لكن قُرب الورم من مراكز اللغة والذاكرة جعل الجراحة محفوفة بالمخاطر. بدأت العائلة في البحث عن بدائل في الخارج - باحثةً عن مركز يجمع بين الابتكار الطبي والنهج الشخصي للرعاية.
ومن خلال Booking Health، تمكنوا من التواصل مع مستشفى متخصص في علاج الأورام العصبية في ألمانيا، حيث اقترح فريق متعدد التخصصات علاج لأورام الدماغ النجمية شخصي مخصص. تضمن جوهر الخطة العلاج بالخلايا المتغصنة Dendritic cell therapy، وهو علاج مناعي متقدم مُصمم لإعادة تدريب جهاز المناعة لدى المريض على التعرف على الخلايا السرطانية ومهاجمتها.
شَمل مسار علاج ماركو ما يلي:
- الاستئصال الدقيق للورم باستخدام التخصيط أثناء الجراحة للحفاظ على الوظيفة الإدراكية
- سلسلة من تطعيمات الخلايا المتغصنة Dendritic cell vaccinations، مصنوعة من مستضدات الورم وخلايا الدم البيضاء الخاصة به
- علاجات مساعدة، بما في ذلك إشعاع حزم البروتونات Proton beam radiation وإعادة التأهيل الشخصي
وعلى عكس الخيارات التقليدية التي تفقد تأثيرها بعد انتهاء العلاج، وفّر العلاج بالخلايا المتغصنة مراقبة مناعية طويلة الأمد. لم تُظهر صور الرنين المغناطيسي للمتابعة على مدى الثمانية عشر شهراً التالية أي علامات على عودة المرض. والأهم من ذلك، عاد ماركو إلى مهنته، واستعاد استقلاليته الكاملة، ولم يُبلغ عن أي خلل عصبي كبير. قال ماركو: "لقد اخترنا مركزاً لم يُعنَ فقط بعلاج الورم، بل عاملوني كإنسان،".
تعكس قصته المشهدَ المتطورَ لعلاج الورم النجمي في ألمانيا حالياً. تكتسب العلاجات المناعية مثل لقاحات الخلايا المتغصنة Dendritic cell vaccines اعترافاً ليس فقط بسبب أُسسها العلمية ولكن أيضاً بسبب جودة الحياة التي تُساعد في الحفاظ عليها.
يستكشف المرضى حول العالم الآن خيارات تتجاوز العلاج التقليدي. وقد برزت ألمانيا، على وجه الخصوص، كمركز رائد في مجال طب الأورام العصبية المتقدم طفيف التوغل - حيث يختار عدد متزايد من المرضى الدوليين مستشفيات لعلاج الورم النجمي تجمع بين الابتكار، والسلامة، والتعاطف الرحيم.
أمل في علاج السرطان: نجاح المرضى مع Booking Health
الورم النجمي في المرحلة المتقدمة: عندما يفشل العلاج القياسي، يُقدم الابتكار أملاً جديداً
إن تشخيص إصابتك بورم متقدم في الدماغ غالباً ما يعطي إحساساً بالنهاية. فبعد عدة جولات علاجية ذات تأثير ضئيل، من الشائع سماع أن الخيارات محدودة. في حالات مثل الورم النجمي من الدرجة 4، قد يبدو المرض خارجاً عن السيطرة. ولكن حتى في هذه المرحلة، يمكن للطب الحديث أن يقدم اتجاهات جديدة.
لقد تغير نهج علاج أورام الدماغ الخبيثة بشكل جذري. فبينما لا تزال البروتوكولات التقليدية تلعب دوراً، إلا أنها لم تعد الخيار الوحيد. بالنسبة لأولئك الذين يواجهون ورم نجمي عالي الدرجة، فإن الاستراتيجيات الشخصية التي تتضمن العلاج الموجه، والإشعاع الدقيق، والطرق المناعية يمكن أن تُحدث فرقاً ملموساً - غالباً مع آثار جانبية أقل ونتائج أفضل.
يعتمد الوصول إلى أفضل خيارات العلاج للورم النجمي في الدماغ الآن على أكثر من مجرد التشخيص نفسه. فعوامل مثل الطفرات الجينية، والاستجابة للعلاج السابق، والصحة العامة تُحدد المسار العلاجي الأكثر فعالية. تُقدم المستشفيات الرائدة في الخارج خطط علاج شاملة وفردية لعلاج الورم النجمي وعلاج الورم الأرومي الدبقي - وبمساعدة Booking Health، يُمكن للمرضى الوصول مباشرةً إلى هذه البرامج دون أي تأخير أو وسطاء غير ضروريين.
حتى عند مواجهة تشخيص خطير مثل المرحلة الرابعة من الورم النجمي، لا يزال هناك مجال لاتخاذ قرارات صائبة. الأمر لا يتعلق بأمل كاذب - بل بمعرفة أين نبحث والتصرف قبل فوات الأوان.
رحلة طبية: كل خطوة على الطريق مع Booking Health
يُعدّ إيجاد أفضل استراتيجية علاج لحالتك السريرية مهمة صعبة. فكونك مستنزَفاً بالفعل من جلسات العلاج المتعددة، واستشارة العديد من المتخصصين، وتجربة مختلف التدخلات العلاجية، قد تشعر بالضياع وسط كل المعلومات التي يقدمها لك الأطباء. في مثل هذه الحالة، من السهل اختيار خيار مباشر، أو اتباع بروتوكولات علاجية موحدة ذات قائمة طويلة من الآثار السلبية بدلاً من اختيار خيارات علاجية مبتكرة عالية التخصص.
لتتمكن من اتخاذ قرار مُستنير والحصول على خطة إدارة السرطان المخصصة لك، والتي سيتم تصميمها لتناسب حالتك السريرية المحددة، استشر الخبراء الطبيين في Booking Health. بفضل ريادتها في تقديم أحدث الابتكارات الطبية على مدار 12 عاماً بالفعل، تتمتع Booking Health بخبرة متينة واسعة في إنشاء برامج إدارة السرطان المعقدة لكل حالة على حدة. وكشركة مرموقة، تقدم Booking Health خطط علاج الأورام النجمية المخصصة الشخصية، مع حجز مباشر للمستشفى ودعم كامل في كل مرحلة، من العمليات التنظيمية إلى المساعدة أثناء العلاج. نحن نقدم:
- تقييم وتحليل التقارير الطبية
- تطوير برنامج الرعاية الطبية
- اختيار مكان العلاج المناسب
- إعداد الوثائق الطبية وإرسالها إلى المستشفى المناسب
- استشارات تحضيرية مع الأطباء لتطوير برامج الرعاية الطبية
- نصائح الخبراء أثناء الإقامة في المستشفى
- رعاية المتابعة بعد عودة المريض إلى بلده الأصلي بعد إتمام برنامج الرعاية الطبية
- الاهتمام بالإجراءات الرسمية كجزء من التحضير لبرنامج الرعاية الطبية
- تنسيق وتنظيم إقامة المريض في بلد أجنبي
- المساعدة في الحصول على التأشيرات وتذاكر السفر
- منسق شخصي ومترجم فوري مع دعم على مدار الساعة 24/7
- ميزانية شفافة بدون أي تكاليف خفية
الصحة جانب لا يُقدّر بثمن في حياتنا. لذا، ينبغي تفويض إدارة شيء هش ولكنه ثمين فقط إلى خبراء ذوي خبرة مُثبتة وسُمعة حسنة. Booking Health شريك موثوق يُساعدك في رحلة حصولك على صحة أقوى وجودة حياة أفضل. اتصل بمستشارنا الطبي لمعرفة المزيد عن إمكانيات العلاج المُخصص الشخصي باستخدام أساليب مُبتكرة لـ الأورام النجمية مع كبار المُتخصصين في هذا المجال.
الأسئلة الشائعة حول الورم النجمي في الدماغ
أرسل طلب للعلاجالورم النجمي Astrocytoma هو ورم الخلايا النجمية في الجهاز العصبي المركزي CNS يُصيب المرضى البالغين والأطفال. يؤثر على وظائف الدماغ حسب موقعه (جذع الدماغ، النخاع الشوكي). يتضمن التشخيص إجراء التصوير بالرنين المغناطيسي MRI والخزعة مع توجيه العلاج من قِبل متخصصي الأورام العصبية.
يمكن أن يكون الورم النجمي حميداً (منخفض الدرجة) أو خبيثاً (عالي الدرجة). يتم تحديد نوع الورم من خلال التصوير بالرنين المغناطيسي MRI والخزعة. غالباً ما يشمل العلاج الجراحة، والعلاج الإشعاعي، والعلاج الكيميائي، اعتماداً على الخباثة.
تشمل الأعراض الصداع، والنوبات، وتشوش الرؤية، واضطرابات عصبية. قد تؤثر الأورام القريبة من جذع الدماغ على الوظائف الحيوية. يستخدم التشخيص التصوير بالرنين المغناطيسي MRI والتصوير المقطعي المحوسب CT، ويراقب أطباء الأعصاب تطور الحالة.
تتراوح الدرجات من الدرجة الأولى (شعري الخلايا، حميد) إلى الدرجة الرابعة (الورم الأرومي الدبقي، خبيث). تؤثر درجة الورم على التوقعات وخيارات العلاج، مثل الجراحة، أو العلاج الإشعاعي أو العلاج الكيميائي.
الورم النجمي الكشمي هو ورم خبيث عالي الدرجة يصيب الجهاز العصبي المركزي CNS ويتطلب جراحة، وعلاج إشعاعي، وعلاج كيميائي. مناقشات مجلس الأورام ترشد العلاج المستهدف ومراقبة التكرار.
الورم النجمي شعري الخلايا هو ورم حميد منخفض الدرجة يُصيب غالباً المرضى الأطفال. يُؤدي الاستئصال الجراحي إلى تعافي جيد وتوقعات مواتية. التصوير بالرنين المغناطيسي MRI والخزعة يؤكدان التشخيص.
تشمل الأسباب الطفرات الجينية والعوامل البيئية كالإشعاع. تتضمن عملية التشخيص والتخطيط للعلاج مشاركة أطباء الأعصاب، وجراحي الأعصاب، وأخصائيي الأورام.
يعتمد البقاء على قيد الحياة على درجة الورم والعلاج. الأورام النجمية منخفضة الدرجة قد تسمح بحياة طويلة مع المراقبة؛ بينما الأنواع عالية الدرجة لها معدلات بقاء على قيد الحياة أقصر على الرغم من الجراحة، والعلاج الإشعاعي، والعلاج الكيميائي.
يختلف متوسط العمر المتوقع: غالباً ما يعيش مرضى الورم النجمي منخفض الدرجة أكثر من عشر سنوات، بينما يبلغ متوسط البقاء على قيد الحياة لمرضى الورم النجمي عالي الدرجة أقل من عامين. يُحسّن التشخيص المبكر والعلاج متعدد الوسائط جودة الحياة.
يشمل التشخيص التصوير بالرنين المغناطيسي MRI، والتصوير المقطعي المحوسب CT، والخزعة لتقييم نوع الورم ودرجته. يُقيِّم أطباء الأعصاب وفرق الأورام العصبية أعراضاً مثل النوبات وعدم وضوح الرؤية.
غالباً ما يمكن شفاء الأورام النجمية منخفضة الدرجة أو السيطرة عليها على المدى الطويل بالجراحة والمراقبة. تتطلب الأورام عالية الدرجة علاجاً مكثفاً؛ والشفاء نادر، لكن العلاج يُحسّن فرص البقاء على قيد الحياة.
يشمل العلاج حج القحف (فتح الجمجمة)، والاستئصال، والعلاج الإشعاعي، والعلاج الكيميائي، والعلاج المناعي. تقوم مجالس الأورام بتصميم العلاج المستهدف وفقاً لاحتياجات المريض لتحسين التوقعات والتعافي.
عادةً ما تكون الجراحة ضرورية لأخذ خزعة وإزالة الورم، ولكن قد تكون محدودة حسب موقع الورم أو حالة المريض. في بعض الحالات، يتم اللجوء إلى المراقبة أو العلاج غير الجراحي.
الورم النجمي من الدرجة الرابعة (الورم الأرومي الدبقي) له توقعات سيئة مع متوسط البقاء على قيد الحياة حوالي 12-18 شهراً على الرغم من الجراحة، والعلاج الإشعاعي، والعلاج الكيميائي.
الورم الأرومي الدبقي Glioblastoma هو ورم نجمي astrocytoma من الدرجة الرابعة، شديد الخباثة وعدواني. في حين أن جميع الأورام الأرومية الدبقية هي أورام نجمية، إلا أنه ليس كل الأورام النجمية أورام أرومية دبقية.
يعتمد معدل البقاء على قيد الحياة على درجة الورم: تُظهر الأورام النجمية منخفضة الدرجة نسبة بقاء على قيد الحياة لمدة خمس سنوات تزيد عن 70٪، بينما الأورام النجمية عالية الدرجة أقل من 20٪. يُعدّ التشخيص المبكر ورعاية الأورام الشاملة أمراً حيوياً بالغ الأهمية.
نعم، ظهر العلاج بالخلايا المتغصنة إلى جانب الجراحة التقليدية، والعلاج الإشعاعي، والعلاج الكيميائي، بهدف تحسين معدلات البقاء على قيد الحياة والحد من تكرار المرض.
تُقدم ألمانيا رعاية متقدمة في مجال الأورام العصبية، مع خبراء في جراحة الأعصاب، والعلاج الإشعاعي، والعلاج الكيميائي، بالإضافة إلى إمكانية الوصول إلى خيارات العلاج المناعي المبتكرة.
ابحث عن فرق متعددة التخصصات، تشمل أطباء الأعصاب، وجراحي الأعصاب، وأطباء الأورام. يساعد المنسق الطبي Booking Health في العثور على أفضل المتخصصين وخطط العلاج الشخصية.
يمكن أن يجمع علاج الورم النجمي Astrocytoma بين الجراحة (Keyhole أو التنظير الداخلي Endoscopic)، والعلاج بالبروتون أو العلاج الإشعاعي، والأساليب المبتكرة مثل العلاج بالخلايا المتغصنة Dendritic cell therapy، والعلاج الكيميائي الكهربائي (ECT)، والعلاج الحراري الخلالي بالليزر (LITT). عادةً، يعتمد الاختيار على درجة الورم وموقعه.
في أوروبا، تتراوح أسعار علاج الورم النجمي من 20.000 € إلى 90.500 €: الجراحة 25.000 € - 50.000 €، والعلاج بالبروتون 56.900 € - 90.500 €، والعلاج بالخلايا المتغصنة 20.000 € - 38.000 €، والعلاج الكيميائي الكهربائي 30.000 € - 45.000 €. على وجه الخصوص، تُقدم ألمانيا رعاية عالية الجودة بأسعار معقولة، بينما تميل بريطانيا العظمى إلى أن تكون أكثر تكلفة. على النقيض من أوروبا، فإن دولاً مثل أستراليا، غالباً ما توفر وصولاً محدوداً إلى العلاجات المتقدمة (مثل العلاج بالخلايا المتغصنة أو العلاج بالبروتون). وحتى عندما تكون متوفرة، يمكن أن تكون التكلفة أعلى بعدة مرات من تكلفتها مقارنةً بالمستشفيات الأوروبية.
يمكن تختلف نتائج علاج الورم النجمي باختلاف الطريقة ودرجة الورم. وبشكل أكثر تحديداً، يمكن للجراحة أن تحقق استجابة بنسبة 60-80٪ في المراحل المبكرة و 20-30٪ في المراحل المتقدمة. في المقابل، يمكن أن تصل نسبة نجاح العلاج بالبروتون إلى 50-70٪ والعلاج بالخلايا المتغصنة إلى 95٪ (في المراحل المبكرة) و 80٪ (في المراحل المتقدمة)، والعلاج الكيميائي الكهربائي إلى حوالي 70٪.
أثناء علاج الورم النجمي، قد يُسبب العلاج الإشعاعي التعب وتغيرات معرفية. من ناحيةً أخرى، يمكن أن يساعد العلاج بالبروتون في تقليل هذه المخاطر. في المقابل، يُسبب العلاج بالخلايا المتغصنة عادةً أعراضاً خفيفة تُشبه أعراض الإنفلونزا، في حين أن ECT و LITT لهما تأثيرات قصيرة المدى وموضعية.
بالنسبة لطرق علاج الورم النجمي، تُعتبر الجراحة و LITT إجراءات لمرة واحدة One-time procedures. في المقابل، يستغرق العلاج بالبروتون والعلاج الإشعاعي عادةً ستة أسابيع. من ناحية أخرى، يتم إكمال العلاج بالخلايا المتغصنة و ECT في جلسة واحدة.
أدت العلاجات الجديدة للورم النجمي إلى تحسين نتائج المرضى. فعلى سبيل المثال، يمكن أن تؤدي إضافة العلاج بالخلايا المتغصنة إلى زيادة معدل البقاء على قيد الحياة لمدة خمس سنوات إلى أكثر من الضعف، ويمكن أن يؤدي ECT إلى إطالة متوسط البقاء على قيد الحياة من 9 إلى 14 شهراً، ويمكن أن يساعد العلاج بالبروتون في الحفاظ على وظيفة الدماغ وجودة الحياة على المدى الطويل.
يُركز أفضل خيار علاج للورم النجمي في الدماغ على التقنيات المبتكرة وطفيفة التوغل، التي توفر مزايا مقارنةً بالعلاج القياسي. في ألمانيا، تشمل الخيارات المتقدمة العلاج الحراري الخلالي بالليزر (LITT)، والعلاج الكيميائي الكهربائي، وانصمام الورم (الذي يسمح بالتحكم المستهدف في الورم مع الحفاظ على أنسجة الدماغ السليمة).
أفضل المستشفيات لعلاج الورم النجمي في الدماغ هي مراكز متخصصة في طب الأورام العصبية وتتمتع بخبرة في الإجراءات المبتكرة. في ألمانيا، توفر هذه المستشفيات إمكانية الوصول إلى العلاج الحراري الخلالي بالليزر (LITT)، والعلاج الكيميائي الكهربائي، والانصمام (بدعم من قبل فرق متعددة التخصصات وتقنيات متقدمة أثناء الجراحة).
اختر العلاج في الخارج وستحصل بالتأكيد على أفضل النتائج!
المؤلفون:
تم تحرير المقال من قبل خبراء طبيين وأطباء معتمدين من مجلس الأطباء الدكتورة ناديجدا إيفانيسوفا و الدكتور بوغدان ميخالنيوك. لعلاج الحالات المشار إليها في المقال، يجب استشارة الطبيب؛ المعلومات الواردة في المقالة ليست مخصصة للتطبيب الذاتي!
سياستنا التحريرية، التي توضح بالتفصيل التزامنا بالدقة والشفافية، متاحة هنا. انقر على هذا الرابط لمراجعة سياساتنا.
المصادر:
[1] Medscape. الورم النجمي: أساسيات الممارسة، والخلفية، والفيزيولوجيا المرضية.
https://emedicine.medscape.com/article/283453-overview
[2] Open Exploration. تحديث بشأن الأورام النجمية: اعتبارات الإدارة الطبية والجراحية.
https://www.explorationpub.com/Journals/en/Article/10069
[3] PubMed. العلاج بالبروتونات للورم الدبقي المنتشر من نوع البالغين: مراجعة منهجية.
https://pubmed.ncbi.nlm.nih.gov/39251047/
[4] PubMed. العلاج بالبروتون المعدل الشدة، والعلاج بالقوس الحجمي المعدل، والعلاج الإشعاعي المطابق ثلاثي الأبعاد في الورم النجمي الكشمي والورم الأرومي الدبقي: مقارنة قياس الجرعات.
https://pubmed.ncbi.nlm.nih.gov/27334276/
[5] PubMed Central. تصعيد جرعة الإشعاع الخارجي للورم الدبقي عالي الدرجة
https://pmc.ncbi.nlm.nih.gov/articles/PMC7389526/
[6] The Nobel Prize. جائزة نوبل في علم وظائف الأعضاء أو الطب 2011، حقائق رالف م. ستاينمان.
https://www.nobelprize.org/prizes/medicine/2011/steinman/facts/
[7] Journal of Translational Medicine. النتائج الأولية للبقاء على قيد الحياة من تجربة سريرية كبيرة في المرحلة الثالثة للقاح الخلايا المتغصنة الذاتية في ورم أرومي دبقي تم تشخيصه حديثاً.
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-018-1507-6
اقرأ:
علاج سرطان الدماغ – الدليل الكامل: جميع خيارات علاج سرطان الدماغ الجديدة
قائمة المقالات:
- طرق العلاج القياسية: الجراحة، والعلاج بالبروتونات، والإشعاع
- إعادة برمجة المناعة: كيف يُسهم العلاج بالخلايا المتغصنة في تشكيل مستقبل رعاية أورام الدماغ
- علاجات جديدة للورم النجمي في الدماغ: تقنيات الأشعة التداخلية
- من التشخيص إلى التعافي
- الورم النجمي في المرحلة المتقدمة: عندما يفشل العلاج القياسي، يُقدم الابتكار أملاً جديداً
- رحلة طبية: كل خطوة على الطريق مع Booking Health
- الأسئلة الشائعة حول الورم النجمي في الدماغ
لا تعرف من أين تبدأ؟
اتصل بـ Booking Health












