سرطان المستقيم هو نوع من السرطان يبدأ في أنسجة المستقيم، الجزء الأخير من الأمعاء الغليظة. على الرغم من تصنيفه في كثير من الأحيان مع سرطان القولون، إلا أن سرطان المستقيم يمثل تحديات فريدة بسبب موقعه بالقرب من هياكل حيوية حرجة، مثل العضلة العاصرة، والمثانة، والأعضاء التناسلية. هذا القرب يجعل التشخيص، والعلاج لسرطان المستقيم، واتخاذ القرارات الجراحية معقداً بشكل خاص. في بعض الحالات، تمتد الأورام من المستقيم إلى القولون السيني، مما قد يتطلب تخطيط علاج مشترك وتصوير دقيق لتحديد النهج الأمثل.
وفقاً لمنظمة الصحة العالمية [1]، يُعد سرطان القولون والمستقيم ثالث أكثر أنواع السرطان شيوعاً حول العالم، وثاني أكبر سبب للوفيات المرتبطة بالسرطان [2]. في ألمانيا وحدها، يتم تشخيص أكثر من 60.000 حالة جديدة من سرطان القولون والمستقيم سنوياً، ثلثها تقريباً يصيب المستقيم [3]. تختلف معدلات البقاء على قيد الحياة بشكلٍ كبير اعتماداً على المرحلة التي يتم فيها اكتشاف السرطان. في حين أن المراحل المبكرة من السرطان (المرحلتان الأولى والثانية) تتجاوز معدلات البقاء على قيد الحياة لمدة خمس سنوات 80٪، فإن المرحلة المتأخرة من المرض، وخاصةً مع النقائل، تُقلل بشكلٍ كبير من فرصة تحقيق هدأة طويلة الأمد [4].
لسوء الحظ، غالباً ما يتطور سرطان المستقيم بصمت. يتم تشخيص العديد من المرضى فقط بعد أن يشهدوا أعراض، مثل النزيف، أو انسداد الأمعاء، أو آلام البطن. هذه هي العلامات التي قد تُشير إلى مرحلة أكثر تقدُماً. على الرغم من التحديات، فإن التطورات في علاج سرطان المستقيم حولت نظرة العديد من المرضى. اليوم، مع التدخل في الوقت المناسب، والعلاجات المبتكرة، والرعاية الفردية، هناك أمل حقيقي. الكثير والكثير من الأشخاص لا ينجون من سرطان المستقيم فحسب، بل يستعيدون صحتهم ويعودون إلى حياة مُرضية.
بروتوكولات العلاج القياسية (المراحل 1-3)
يعتمد اختيار العلاج لسرطان المستقيم المبكر والمتقدم موضعياً على مرحلة المرض، وموقع الورم، والصحة العامة للمريض. وفقاً لـ المبادئ التوجيهية لعلاج سرطان المستقيم الدولية، فإن علاج المرحلة الأولى من سرطان المستقيم ينطوي عادةً على الإزالة الجراحية للورم. في كثير من الحالات، يتم إجراء استئصال طفيف التوغل بالتنظير البطني أو الاستئصال بالروبوت Robotic resection، مما يسمح بالتعافي السريع والحفاظ على وظيفة الأمعاء الطبيعية. عندما تكون الأورام صغيرة ومحددة جيداً، فإن هذا العلاج للمرحلة 1 من سرطان المستقيم غالباً ما يقضي على الحاجة لعلاجات إضافية لعلاج سرطان المستقيم في المرحلة الاولى.
بالنسبة لعلاج المرحلة الثانية من سرطان المستقيم، فإن النهج القياسي عادةً ما يجمع بين العلاج المساعد الجديد، وهو غالباً العلاج الكيميائي الإشعاعي، متبوعاً بالجراحة. الهدف من علاج ما قبل العملية هو تقليص الورم وزيادة احتمالية الإزالة الكاملة مع تقليل خطر تكراره موضعياً. يمكن للجراحة بعد العلاج المساعد الجديد في كثير من الأحيان تجنُب الحاجة إلى الفغر، وخاصةً في الأورام التي تقع أعلى المستقيم.
يتضمن علاج المرحلة الثالثة من سرطان المستقيم استراتيجية أكثر عدوانية بسبب تورط العقد اللمفاوية. يتلقى المرضى عادةً العلاج الكيميائي والعلاج الإشعاعي قبل الجراحة لتقليل عبء الورم. بعد الجراحة، يتم إعطاء العلاج الكيميائي المساعد للقضاء على أي مرض مجهري متبقي. كلما كان ذلك ممكناً، يتم إعطاء الأولوية لـ الإجراءات المحافظة على العضلة العاصرة للحفاظ على جودة الحياة دون المساس بالسلامة من الأورام. عندما تكون الأورام منخفضة في المستقيم أو تُسبب انسداداً شديداً، قد يكون فغر القولون ضرورياً، ومؤقتاً أو دائماً، للسماح بوظيفة الأمعاء الطبيعية أو للشفاء بعد الجراحة. بشكلٍ عام، فإن العلاج للمرحلة الثالثة من سرطان المستقيم عادةً ما يجمع بين عدة أساليب ويجب أن يعالج كلا من الورم الأساسي والعقد اللمفاوية الإقليمية لتحسين النتائج على المدى الطويل.
قيود الأساليب التقليدية
في حين تظل العلاجات القياسية تُشكل الأساس لرعاية سرطان المستقيم، إلا أنها ليست خالية من التحديات الكبيرة. العديد من المرضى، حتى بعد الخضوع للجراحة، والعلاج الكيميائي، والعلاج الإشعاعي، يواجهون خطر تكرار المرض أو انتشاره في النهاية إلى الكبد، أو الرئتين، أو العقد اللمفاوية. في هذه الحالات، تنخفض معدلات البقاء على قيد الحياة بشكلٍ حاد، وتضيق نافذة العلاج الشافي لسرطان المستقيم.
علاوةً على ذلك، قد يكون من الصعب تحمل الآثار الجانبية للعلاجات التقليدية. غالباً ما يُبلغ المرضى عن خلل وظيفي مزمن في الأمعاء، وألم، وتعب، ونزيف، وانخفاض جودة الحياة. فترات العلاج الطويلة، والزيارات المتكررة للمستشفى، ومضاعفات ما بعد الجراحة يمكن أن تُسبب المزيد من العبء الجسدي والنفسي. تؤثر هذه التحديات بشكلٍ كبير على توقعات المريض على المدى الطويل، خاصةً عندما تُصبح الأورام مقاومة للعلاجات التقليدية أو تتكرر بعد الجراحة.
الأساليب الجديدة والمبتكرة
مع استمرار تطور العلوم الطبية، أصبح بإمكان المرضى اليوم الوصول إلى مجموعة من العلاجات الجديدة لسرطان المستقيم والتي تتجاوز بكثير البروتوكولات التقليدية. لا تهدف هذه الأساليب إلى إطالة البقاء على قيد الحياة فحسب، بل تهدف أيضاً إلى تقليل الآثار الجانبية وتحسين جودة الحياة.
من بين هذه التطورات العلاجات الموجهة التي تُعطّل نمو السرطان على المستوى الجزيئي وتقنيات العلاج المناعي التي تعمل على تمكين جهاز المناعة في الجسم من مكافحة الأورام الخبيثة. في كثير من الحالات، يمكن استخدام هذه الخيارات بالاشتراك مع العلاجات التقليدية، مثل العلاج الكيميائي والعلاج الإشعاعي، مما يُزيد من فعاليتها. بفضل الأدوات الروبوتية وأدوات التنظير البطني التي تسمح بدقة أكبر وأوقات تعافي أسرع، حتى الجراحة أصبحت أقل غزواً.
بالنسبة للمرضى الذين يسعون لـ العلاج البديل لسرطان المستقيم أو استنفدوا الخيارات التقليدية، فإن هذه الأساليب الجديدة لا توفر حياة أطول فحسب بل توفر أيضاً مساراً أكثر كرامة وراحة خلال العلاج. في بعض الحالات، يُحقق المرضى استقرار المرض أو الهدأة مع مضاعفات أقل بكثير من تلك المرتبطة بالعلاجات التقليدية.
العلاج بالخلايا المتغصنة
أحد التطورات في علاج سرطان المستقيم بدون جراحة الحديث هو العلاج بالخلايا المتغصنة Dendritic cell therapy. هذا شكل من أشكال العلاج المناعي الذي يستخدم قوة جهاز المناعة في الجسم لمكافحة السرطان. يستهدف هذا النهج المبتكر المرض من جذوره عن طريق تدريب الخلايا المناعية للتعرف على خلايا الورم وتدميرها.
تُعرف الخلايا المتغصنة بأنها "الحُراس" في جهاز المناعة. دورها الرئيسي هو اكتشاف التهديدات، والتقاط المستضدات الغريبة، وتقديمها إلى الخلايا التائية T cells، مما يُحفز استجابة مناعية موجهة. في العلاج بالخلايا المتغصنة، تُستخرج الخلايا المتغصنة من المريض من خلال سحب بسيط للدم، ثم تُعرَّض لعينات خزعة السرطان في المختبر. بمجرد "تدريبها" للتعرف على العلامات الخاصة بالورم، يتم إعادة إدخال هذه الخلايا إلى جسم المريض، حيث تعمل على تحفيز الخلايا التائية T cells لتحديد موقع السرطان ومهاجمته.
اكتسبت هذه الطريقة شهرة عالمية بعد أن طرح الدكتور رالف ستاينمان، الحائز على جائزة نوبل، مفهوم العلاج القائم على الخلايا المتغصنة [5]. ومنذ ذلك الحين، أصبح هذا العلاج أحد أفضل العلاجات لسرطان المستقيم، وخاصةً للمرضى الذين يعانون من نقائل أو أولئك الذين يبحثون عن خيار غير جراحي. على عكس العلاج الكيميائي أو علاج سرطان المستقيم بالاشعاع، فإن العلاج المتغصن لا يُلحق الضرر بالأنسجة السليمة وجيد التحمل عموماً مع آثار جانبية قليلة.
الأشعة التداخلية
الأشعة التداخلية (IR) تعمل على تحويل كيفية تعاملنا مع خيارات علاج سرطان المستقيم، وخاصةً في الحالات المعقدة أو المتقدمة. يجمع هذا المجال طفيف التوغل بين التصوير المتقدم، مثل التصوير المقطعي المحوسب CT، و PET/CT، والتصوير بالرنين المغناطيسي MRI، مع علاجات موجهة تُدمر الأورام بدقة، وغالباً دون الحاجة إلى جراحة مفتوحة. تُستخدم تقنيات IR الآن بشكل متكرر كجزء من علاج سرطان المستقيم في المرحلة 3 لتخفيف الانسداد، أو السيطرة على النزيف، أو تقليص الأورام عندما لا تكون الطرق التقليدية كافية. تُصبح هذه التقنيات جزءاً من أفضل علاج لسرطان المستقيم بشكل متزايد، خاصةً عندما تفشل الخيارات القياسية.
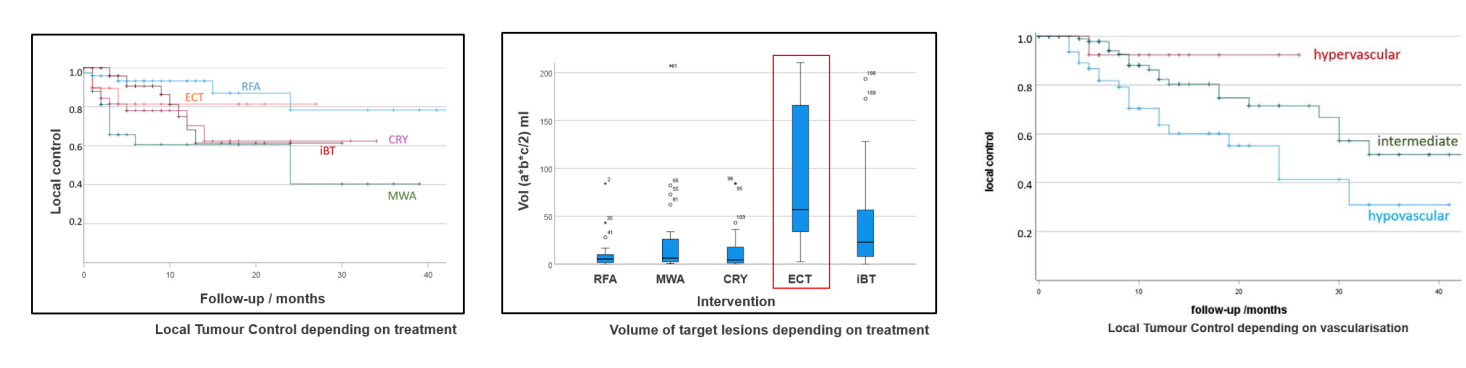
الاجتثاث الحراري، بما في ذلك الاجتثاث بالترددات الراديوية (RFA) والاجتثاث بالميكروويف (MWA)، يستخدم الحرارة لتدمير الأنسجة السرطانية. يُعتبر فعال بشكلٍ خاص في علاج نقائل القولون والمستقيم في الكبد أو الحوض [6]. وجدت دراسة استباقية حديثة أن الاجتثاث الحراري بالاشتراك مع العلاج الكيميائي يحقق سيطرة موضعية على الورم في ما يصل إلى 80٪ من المرضى في عام واحد، مع تمديد البقاء على قيد الحياة الخالي من تقدُم المرض لمدة 4-8 أشهر لأولئك الذين يعانون من مرض نقيلي محدود. يُعد MWA مفيداً بشكل خاص في المناطق ذات الأورام الكبيرة أو التشريح المعقد، إذ يُنشئ مناطق اجتثاث أكبر وأسرع مقارنةً بـ RFA. يتم تنفيذ هذه الإجراءات عادةً باستخدام التوجية بالتصوير وعن طريق الجلد، ولا تتطلب سوى إقامة قصيرة في المستشفى وتوفر وقت تعافي قصير.
الاجتثاث بالتبريد يجمد خلايا الورم بسرعة، مُسبباً تكوين بلورات ثلجية تدمر الورم وإمداده بالدم. هذه التقنية مفيدة بشكلٍ خاص للأورام الموجودة بالقرب من الهياكل الحساسة، مثل المثانة أو الأعصاب. أظهرت دراسة متعددة المراكز استقرار المرض في 67-70٪ من المرضى الذين يعانون من تكرار أمراض الحوض غير القابلة للاستئصال، جنباً إلى جنب مع تخفيف كبير لآلام الأمعاء وأعراض المسالك البولية. غالباً ما يتم تفضيل هذه التقنية عندما تُشكل الطرق الحرارية مخاطر على الهياكل المجاورة، حيث يمكن التحكم في عملية التجميد والذوبان بعناية. يمكن أيضاً تكرار الاجتثاث بالتبريد إذا لزم الأمر، مما يجعله أداة مرنة في إدارة الورم على المدى الطويل.
عندما يعجز العلاج الكيميائي عن اختراق الخلايا السرطانية: التثقيب الكهربائي هو الحل
العلاج الكيميائي الكهربائي (ECT) يجمع بين النبضات الكهربائية الموضعية والعلاج الكيميائي لتعزيز امتصاص الدواء في خلايا الورم. على الرغم من أن ECT لا يزال تجريبياً في علاج سرطان المستقيم، إلا أنه أظهر معدلات استجابة تصل إلى 68٪، حتى لدى المرضى الذين تلقوا علاجاً مكثفاً مسبقاً. قد يعمل أيضاً على تحفيز استجابات مناعية موضعية، مما يجعله رفيقاً محتملاً للعلاج المناعي. يُعد ECT مفيداً للغاية في حالات تكرار الورم السطحي أو العجاني ويمكن تطبيقه تحت التخدير الموضعي أو العام اعتماداً على موقع الورم. نظراُ لسُميته الجهازية المنخفضة، يتم تحمله بشكلٍ جيد حتى من قِبل كبار السن أو المرضى الضعفاء.
التثقيب الكهربائي غير المعكوس (IRE) هو تقنية غير حرارية تستخدم نبضات كهربائية مكثفة لتدمير أغشية الخلايا السرطانية دون الإضرار بالأوعية الدموية أو الأعصاب المحيطة [7]. تُظهر البيانات الحديثة أن معدل البقاء على قيد الحياة الخالي من تقدُم المرض يصل إلى 10.3 أشهر، ومعدلات السيطرة الموضعية تتراوح من 65٪ إلى 80٪ في حالات تكرار سرطان المستقيم التي عولجت باستخدام IRE. يُعتبر هذا الإجراء مثالياً للأورام في المناطق الصعبة تشريحياً، مثل تلك القريبة من الضفيرة العجزية، أو الأوعية الدموية الكبرى، أو الحالبين. يحافظ IRE أيضاً على السلامة الهيكلية للأنسجة، مما يجعله مفيداً عندما قد تكون هناك حاجة إلى تدخلات مستقبلية. يمكن تكراره بأمان ويُستخدم غالباً مع علاجات أخرى، مثل العلاج الكيميائي الجهازي أو العلاج الإشعاعي.
الانصمام الشرياني (AE) هو إجراء طفيف التوغل يُستخدم لقطع إمداد الدم المُغذي للورم، مما يؤدي إلى انكماش الورم أو استقراره. يُعد هذا العلاج مفيداً جداً للمرضى الذين يعانون من نزيف، أو آلام الحوض، أو أورام غير قابلة للجراحة أو العلاج الكيميائي الجهازي. على عكس الانصمام الكيميائي عبر الشرايين (TACE)، لا يقوم AE بتوصيل أي أدوية ولكنه يركز فقط على سد الأوعية باستخدام جزيئات أو ملفات صغيرة. تُشير الدراسات السريرية إلى معدلات سيطرة على النزيف بنسبة 90-95٪ وتخفيف الألم لدى 70-80٪ من المرضى، غالباً في غضون أيام قليلة. يتم استخدام AE بشكل متكرر في خطط العلاج التلطيفي، وخاصةً بالنسبة لأولئك الذين يعانون من سرطان المستقيم المتقدم أو النقيلي والذين يحتاجون إلى رعاية مُركزة على الأعراض دون آثار جانبية كبيرة.
من بين العلاجات الموجهة الأكثر تقدماً المتاحة اليوم، يتميز الانصمام الكيميائي عبر الشرايين (TACE) بقدرته على علاج نقائل سرطان القولون والمستقيم بطريقة موضعية وفعالة للغاية. يعمل TACE على توصيل العلاج الكيميائي مباشرةً إلى الشريان المُغذي للورم، يليه حقن عوامل صِمية تمنع تدفق الدم. يؤدي هذا النهج إلى تجويع الورم مع زيادة تركيز الدواء في الأنسجة السرطانية إلى أقصى حد وتقليل تعرض باقي أجزاء الجسم له.
يُعد TACE ذي قيمة عند حدوث نقائل في الكبد أو الرئتين، وهي مواقع شائعة لانتشار سرطان المستقيم المتقدم. في هذه الحالات، قد لا تكون العلاجات الجهازية القياسية كافية. يسمح TACE لأطباء الأورام التداخلية بعزل هذه النقائل وعلاجها بعدوانية دون إخضاع الجسم بأكمله لجرعات عالية من العلاج الكيميائي.
أظهرت الدراسات أن TACE يمكن أن يُحقق معدلات استجابة تتراوح بين 45-65٪، حيث يشهد بعض المرضى انكماش الورم مما يجعل الجراحة أو الاجتثاث ممكناً. في المرضى الذين يعانون من نقائل معزولة في الكبد، تم توثيق فترات بقاء على قيد الحياة خالية من تقدُم المرض من 8 إلى 12 شهراً، حتى بعد فشل العلاجات التقليدية.
| نوع العلاج | معدل البقاء على قيد الحياة لمدة عامين | معدل الاستجابة | المدة | الآثار الجانبية |
|---|---|---|---|---|
| العلاج القياسي | ~٪25 للسرطان المتقدم | أقل من 10٪ | عدة دورات | شديدة (غثيان، وتعب، وتساقط الشعر، وكبت المناعة، وتهيُج الجلد) |
| الأساليب المبتكرة | ~٪60 للسرطان المتقدم | ٪65-45 | ما يصل إلى 4 جلسات | خفيفة (شعور موضعي بعدم الارتياح) |
* بيانات Booking Health
تكاليف الإجراءات الطبية حول العالم لعلاج سرطان المستقيم
| طريقة العلاج | ألمانيا | بريطانيا العظمى | الولايات المتحدة الأمريكية |
|---|---|---|---|
| العلاج القياسي | 80.000 € - 150.000 € دورة كاملة | 90.000 € - 165.000 € دورة كاملة | 100.000 € - 180.000 € دورة كاملة |
| الأساليب المبتكرة | 25.000 € - 60.000 € دورة كاملة | 70.000 € - 120.000 € دورة كاملة | 100.000 € - 150.000 € دورة كاملة |
* قد تختلف الأسعار اعتماداً على دورة العلاج وخصائص الورم
قصة مريضة: رحلة مارتا نحو التعافي
مارتا زيلينسكا، مُعلمة لغات تبلغ من العمر 58 عاماً من بولندا، تم تشخيصها بالمرحلة الثالثة من سرطان المستقيم بعد أن شهدت تعب غير مُبرر لأشهر، ونزيف المستقيم المتقطع، وتغيرات في عادات الأمعاء لديها. كان تشخيصها الأولي بمثابة صدمة. رغم نمط حياتها النشط والتزامها بالفحوصات الصحية، فوتت تنظير القولون الروتيني أثناء جائحة كورونا. سمح هذا التأخير للورم بالنمو دون أن يتم اكتشافه.
خضعت لعلاج كيميائي إشعاعي قياسي متبوعاً بجراحة. على الرغم من أن الإجراء نجح في إزالة الورم الرئيسي، إلا أن فحوصات ما بعد الجراحة التي أجرتها مارتا كشفت عن وجود نقائل صغيرة ولكنها مثيرة للقلق في كبدها. حذر طبيب الأورام الخاص بها من أنه على الرغم من تطبيق أفضل رعاية تقليدية، إلا أن السرطان قد بدأ بالفعل في الانتشار.
نظراً لكونها غير راغبة في الاكتفاء بالخيارات المحدودة المتاحة في المستشفى المحلي الخاص بها، لجأت مارتا إلى Booking Health للحصول على الدعم. بفضل إرشادهم، تم تحويلها إلى مستشفى ألماني رائد، حيث عُرضت عليها خطة شخصية تضمنت العلاج بالخلايا المتغصنة Dendritic cell therapy لتعزيز استجابتها المناعية و TACE لاستهداف نقائل الكبد بشكلٍ مباشر.
بعد ثلاث دورات من TACE، أظهر التصوير انخفاضاً كبيراً في آفات الكبد. أدت إضافة العلاج المناعي بالخلايا المتغصنة إلى استقرار حالتها بشكلٍ أكبر، مع تحسُن علامات الدم بشكل مُطرد. أفادت مارتا بحدوث آثار جانبية طفيفة جداً وعدم حدوث أي اضطراب في روتينها اليومي. ولأول مرة منذ أشهر، شعرت بالقدرة على السيطرة على صحتها.
الآن، وبعد مرور أكثر من عام، أصبحت مارتا في حالة هدأة جزئية وتستمتع بحياتها مرة أخرى. عادت إلى التدريس بدوام جزئي، وتتحدث بحرية وانفتاح عن رحلتها العلاجية. "لم يُنقذ العلاج حياتي فحسب،" كما تقول. "بل أعاد لي أيضاً قوتي مرة أخرى."
علاج السرطان المتقدم: قصص نجاح المرضى مع Booking Health
أمل ما بعد المرحلة: إدارة الحالات المتقدمة والنهائية
غالباً ما يجلب تشخيص سرطان المستقيم النقيلي أو المتقدم إرهاقاً نفسياً وشعوراً بالنهاية. قد يسمع المرضى عبارات مثل "خياراتك محدودة" أو "المرض قد تقدم بشكلِ كبير." ومع ذلك، حتى في هذه اللحظات، لا يزال هناك طريق للمُضي قدماً. يتطور الطب الحديث بسرعة كبيرة، ولم تعد علاجات اليوم تقتصر على البروتوكولات القياسية فقط.
الأساليب المبتكرة، مثل العلاج المناعي بالخلايا المتغصنة، والانصمام الكيميائي، وتقنيات الإشعاع الموجه، تُقدم الأمل للمرضى الذين قيل لهم ذات يوم إنه لا يوجد أمل لديهم. تعمل هذه العلاجات عن طريق استهداف الأورام بشكلٍ مباشر، وإبطاء تقدُم المرض، وتخفيف الألم، وتقليل عبء الآثار الجانبية. يتم إجراء العديد من هذه العلاجات في العيادات الخارجية Outpatient-based، وهي طفيفة التوغل، ومُصممة خصيصاً لتلبية احتياجات كل فرد. وهذا يثبت أنه حتى في المراحل المتأخرة يمكن أن تكون الرعاية مانحة ومُعززة للحياة.
عندما يتعلق الأمر بعلاج المرحلة 4 من سرطان المستقيم، يكمُن النجاح في بناء استراتيجية علاج فردية تجمع بين التقنيات التقليدية والحديثة. من خلال التركيز على الاستقرار، والراحة، وجودة الحياة، يمكن للمرضى تحقيق معدلات بقاء مُحسنة على قيد الحياة حتى في مواجهة تكرار المرض.
في Booking Health، نحن متخصصون في إيصال المرضى بخبراء رائدين في رعاية السرطان المتكاملة. معاً، نساعدك في العثور على الحلول الصحيحة، لأن عدم التشخيص يعني نهاية الأمل.
Booking Health: شريكك في رعاية السرطان الشخصية
يُعد العثور على الاستراتيجية الصحيحة لإدارة سرطان المستقيم، وخاصةً بعد تشخيص صعب أو علاجات سابقة فاشلة، ليس بالأمر السهل أبداً. يشعر العديد من المرضى بالإرهاق بسبب النصائح الطبية المتضاربة، أو الوصول المحدود إلى العلاجات المبتكرة، أو ببساطة يشعرون بالإرهاق من البروتوكولات القياسية التي لم تعد تُحقق نتائج ذات معنى. في هذه اللحظات، يُصبح من الضروري البحث عن وجهة نظر جديدة مستوحاة من الخبراء. هذا هو المكان الذي يأتي فيه دور Booking Health.
كمُسهل عالمي رائد في السياحة العلاجية مع ما يزيد عن 12 عاماً من الخبرة، تتخصص Booking Health في تنظيم برامج علاج السرطان الشخصية، بما في ذلك الوصول إلى علاج سرطان المستقيم المتقدم حسب المرحلة في ألمانيا. سواءً كنت تبحث عن أفضل مستشفى لعلاج سرطان المستقيم في ألمانيا أو إحدي الدول المتقدمة، أو تسعى للحصول على رأي ثانٍ من أحد أفضل أطباء المستقيم، أو تبحث في علاجات جديدة مثل العلاج المناعي بالخلايا المُتغصنة أو الانصمام الكيميائي، فإننا نعمل على إيصالك بأفضل المتخصصين والمستشفيات في العالم.
نحن نُقدم الدعم الكامل طوال رحلتك العلاجية، بما في ذلك:
- تقييم وتحليل سجلاتك الطبية
- تطوير برنامج علاج فردي
- اختيار المستشفى الأنسب حسب حالتك
- إعداد وإرسال جميع الوثائق الطبية بشكلٍ آمن
- استشارات ما قبل العلاج مع أطباء متخصصين
- التوجيه الاحترافي أثناء إقامتك في المستشفى
- تنسيق رعاية المتابعة بعد العلاج في الوطن الأصلي
- التعامل مع جميع الإجراءات واللوجستيات
- دعم التأشيرات، وحجز رحلات الطيران، وترتيبات الإقامة
- المُساعدة من مُنسق طبي شخصي ومترجم فوري متاح على مدار الساعة 24/7
- ميزانية شفافة بدون تكاليف خفية
صحتك هي من أغلى ما تملك، لذا من الضروري أن توكلها إلى الأشخاص ذوي الخبرة المُثبتة. تضمن لك Booking Health الحصول على رعاية إنسانية عطوفة مُصممة خصيصاً لحالتك، وتوفر الراحة والحلول المتقدمة عندما تكون في أمس الحاجة إليها.
الأسئلة الشائعة لمرضانا حول علاج سرطان المستقيم
أرسل طلب للعلاجعلاج سرطان المستقيم القياسي يشمل الجراحة، والعلاج الكيميائي، والعلاج الإشعاعي. يتم استخدام العلاجات المبتكرة أيضاً بشكل متزايد، مثل العلاج المناعي والأشعة التداخلية.
يتضمن التشخيص عادةً إجراء تنظير القولون، والتصوير (التصوير بالرنين المغناطيسي MRI، والتصوير المقطعي المحوسب CT)، وخزعة الأنسجة لتأكيد الورم الخبيث وتحديد مرحلته.
على الرغم من أن كلاهما يقع ضمن سرطان القولون والمستقيم، إلا أن علاج سرطان المستقيم غالباً ما يتطلب طرقاً أكثر دقة بسبب موقع المستقيم بالقرب من هياكل حرجة.
ليس دائماً. بعض الحالات تستجيب لعلاج سرطان المستقيم بدون جراحة، خاصةً عند استخدام علاجات مبتكرة.
يمكن أن تشمل هذه الأعراض التعب، واختلال وظائف الأمعاء، والألم، وقمع المناعة، اعتماداً على نوع العلاج المُستخدم.
نعم، يمكن لتقنيات مثل الانصمام الكيميائي، والعلاج المناعي، والعلاج الإشعاعي أن تساعد في إدارة أو تقليل الأورام بطريقة غير جراحية.
على الرغم من أن العلاج الكيميائي يمكن أن يكون له آثار جانبية كبيرة، إلا أنه غالباً ما يكون فعالاً، وخاصةً عندما يقترن بالجراحة أو العلاج الإشعاعي.
علاج سرطان المستقيم بالاشعاع يساعد على تقليص الأورام قبل الجراحة وتخفيف الأعراض في الحالات المتقدمة.
تختلف معدلات البقاء على قيد الحياة حسب المرحلة: أكثر من 80٪ للمرحلة المبكرة وحوالي 12-14٪ للمرحلة الرابعة.
في كثير من الأحيان يستخدم الأطباء مزيجاً من الجراحة، والعلاج الكيميائي الإشعاعي، والعلاجات المبتكرة، مثل TACE أو العلاج بالخلايا المتغصنة Dendritic cell therapy.
نعم. علاج سرطان المستقيم الجديد يتضمن العلاج الموجه، والعلاج المناعي، والطرق الإشعاعية طفيفة التوغل.
يُشير إلى العلاج الكيميائي أو العلاج الإشعاعي الذي يتم إعطاؤه قبل الجراحة لتقليص حجم الورم.
من عدة أسابيع إلى أشهر، اعتماداً على المرحلة ونهج العلاج.
نعم. التكرار ممكن، وهذا هو السبب في أن رعاية المتابعة المنتظمة أمر ضروري.
أفضل علاج لسرطان المستقيم بدون فغرة دائمة يجمع بين العلاج المناعي بالخلايا المتغصنة وتقنيات الأشعة التداخلية. تحقق علاجات سرطان المستقيم الحديثة طفيفة التوغل معدلات استجابة من 45٪ إلى 65٪ مع الحفاظ على وظيفة العضلة العاصرة وتجنب فغر القولون الدائم.
نعم، تتضمن خطة العلاج الحديثة لسرطان المستقيم المتقدم موضعياً العلاج المساعد الجديد متبوعاً بالجراحة المحافظة على العضلة العاصرة. يمكن للطرق المبتكرة مثل TACE والاجتثاث الحراري تقليص الأورام، مما يجعل الخيارات الجراحية الخالية من الفغرة ممكنة في العديد من الحالات.
لا، خيارات العلاج غير الجراحية لسرطان المستقيم تشمل العلاج بالخلايا المتغصنة، و TACE، والاجتثاث الحراري، والعلاج الكيميائي الكهربائي. توفر هذه التقنيات طفيفة التوغل سيطرة فعالة على الورم دون تدخل جراحي كبير، خاصةً في الحالات المعقدة.
أحدث العلاجات تتضمن علاج سرطان المستقيم بالعلاج المناعي في MSI-H وأنواع أخرى من الورم، والعلاج بالخلايا المتغصنة، وتقنيات الأشعة التداخلية. يضمن اختيار أفضل مكان لعلاج سرطان المستقيم في أوروبا إمكانية الوصول إلى هذه الأساليب المبتكرة مع نتائج ممتازة.
نعم، علاج سرطان المستقيم بدون خيارات العلاج الكيميائي يشمل العلاج المناعي بالخلايا المتغصنة، والاجتثاث الحراري، والاجتثاث بالتبريد، و TACE.توفر هذه البدائل سيطرة فعالة على الورم مع تجنب الآثار الجانبية الشديدة المرتبطة بأنظمة العلاج الكيميائي التقليدية.
تُظهر تكلفة جراحة سرطان المستقيم في ألمانيا مقابل الولايات المتحدة الأمريكية اختلافات كبيرة. تُقدم ألمانيا أساليب مبتكرة بتكلفة تتراوح من 25.000 € إلى 60.000 € مقابل 80.000 € - 150.000 € للعلاج القياسي، في حين تصل التكاليف في الولايات المتحدة إلى 100.000 € - 180.000 € للرعاية الشاملة.
بالنسبة لسرطان المستقيم المتقدم، يوفر العلاج الجهازي القياسي غالباً معدل بقاء على قيد الحياة لمدة عامين بنسبة 25٪ تقريباً. من ناحيةً أخرى، فإن الأساليب العلاجية المبتكرة (مثل العلاج بالخلايا المتغصنة Dendritic cell therapy و TACE والاجتثاث بالترددات الراديوية / الاجتثاث بالميكروويف والعلاج الكيميائي الكهربائي Electrochemotherapy والتثقيب الكهربائي غير المعكوس IRE) يمكن أن تُساعد في الوصول إلى البقاء على قيد الحياة لمدة عامين بنسبة ~60٪ لدى بعض المرضى.
في سرطان المستقيم Rectal cancer غالباً ما يُحقق العلاج الكيميائي القياسي معدل استجابة <10٪ في المراحل المتقدمة. ومع ذلك، فالخيارات العلاجية المبتكرة (مثل العلاج بالخلايا المتغصنة و TACE والاجتثاث الحراري والعلاج الكيميائي الكهربائي ECT / التثقيب الكهربائي غير المعكوس IRE) يمكن أن تصل إلى معدل استجابة يتراوح بين ~45-65٪ في حالات مُختارة بشكلٍ مناسب.
تتضمن الرعاية القياسية لسرطان المستقيم عدة دورات من العلاج على مدى أشهر. في المقابل، فإن العلاجات المبتكرة (مثل TACE و RFA / MWA و ECT والعلاج بالخلايا المتغصنة) يتم تقديمها عادةً في مجموعات – غالباً ما تصل إلى 4 جلسات – مع فترات إقامة قصيرة في المستشفى أو زيارات في العيادات الخارجية Outpatient visits.
في سرطان المستقيم، يركز العلاج القياسي على السيطرة على المرض لكن غالباً ما تكون الاستجابة متواضعة، وتتطلب دورات علاج أطول وأكثر كثافة. في المقابل، فإن الأساليب العلاجية المبتكرة (مثل الاجتثاث الموجه بالصور، والانصمام الكيميائي داخل الشرايين، والعلاج المناعي) تهدف إلى تحقيق سيطرة / استجابة موضعية أعلى (≈45-65٪) ودورة علاج أقصر تعتمد على الجلسات.
ما هي التكاليف النموذجية لرعاية سرطان المستقيم حسب الدولة (وماذا عن إمكانية الوصول / التكاليف في أستراليا)؟
بالنسبة لرعاية سرطان المستقيم في الخارج، تتراوح التكاليف الإجمالية عادةً: ألمانيا (حوالي 80.000 € - 150.000 € للرعاية القياسية؛ وحوالي 25.000 € - 60.000 € للرعاية المبتكرة)، وبريطانيا العظمى (حوالي 90.000 € - 165.000 € للرعاية القياسية؛ وحوالي 70.000 € - 120.000 € للرعاية المبتكرة)، والولايات المتحدة الأمريكية (حوالي 100.000 € - 180.000 € للرعاية القياسية؛ وحوالي 100.000 € - 150.000 € للرعاية المبتكرة). أما في أستراليا، فيمكن أن يكون الوصول إلى العديد من الخيارات المبتكرة محدود ومُكلف نسبياً.
المستشفى الأمثل هو الذي يتمتع بخبرة في طب الأورام المتقدم (وإمكانية الوصول إلى العلاجات المبتكرة). تستطيع مراكز السرطان الألمانية دمج الأشعة التداخلية مع الأساليب القائمة على المناعية (مثل العلاج بالخلايا المتغصنة) – مما يسمح بتخطيط العلاج الفردي بناءً على سلوك الورم وحالة المريض.
اختر العلاج في الخارج وستحصل بالتأكيد على أفضل النتائج!
المؤلفون:
تم تحرير المقال من قبل خبراء طبيين وأطباء معتمدين من مجلس الأطباء الدكتورة ناديجدا إيفانيسوفا و الدكتور بوغدان ميخالنيوك. لعلاج الحالات المشار إليها في المقال، يجب استشارة الطبيب؛ المعلومات الواردة في المقالة ليست مخصصة للتطبيب الذاتي!
سياستنا التحريرية، التي توضح بالتفصيل التزامنا بالدقة والشفافية، متاحة هنا. انقر على هذا الرابط لمراجعة سياساتنا.
المصادر:
[1] World Health Organization.
https://www.who.int/
[2] Science Direct. سرطان القولون والمستقيم: مشكلة صحية واقتصادية.
https://www.sciencedirect.com/science/article/abs/pii/S1521691823000197
[3] PubMed Central. الرعاية اللامركزية لسرطان القولون والمستقيم في ألمانيا خلال العقد الماضي ارتبطت بارتفاع معدلات المرض والوفيات في المستشفى.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6419594/
[4] National Cancer Control Indicators. البقاء على قيد الحياة النسبي حسب المرحلة عند التشخيص (سرطان القولون والمستقيم).
https://ncci.canceraustralia.gov.au/outcomes/relative-survival-rate/relative-survival-stage-diagnosis-colorectal-cancer
[5] PubMed. جائزة نوبل في علم وظائف الأعضاء أو الطب لعام 2011.
https://pubmed.ncbi.nlm.nih.gov/22053831/
[6] PubMed Central. الاجتثاث بالترددات الراديوية والاجتثاث بالميكروويف مقارنةً بالعلاج الكيميائي الجهازي واستئصال الكبد الجزئي في علاج نقائل الكبد من القولون والمستقيم: مراجعة منهجية وتحليل تلوي.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6021475/
[7] PubMed. التثقيب الكهربائي غير المعكوس لعلاج نقائل الكبد من سرطان القولون والمستقيم: مراجعة.
https://pubmed.ncbi.nlm.nih.gov/35469520/
اقرأ:
علاج المرحلة الرابعة من سرطان القولون في ألمانيا
العلاج بالخلايا المتغصنة في علاج السرطان في ألمانيا - التطعيم ضد السرطان
قائمة المقالات:
لا تعرف من أين تبدأ؟
اتصل بـ Booking Health