يؤثر التهاب المفصل التنكسي (الفصال العظمي) على ملايين الأشخاص حول العالم، مُسبباً الألم وتقييد الحركة، وغالباً ما توفر العلاجات التقليدية راحة مؤقتة فقط. يمثل الانصمام الشرياني (AE) نهجاً رائداً يستهدف المكون الوعائي لالتهاب المفصل. يقوم هذا الإجراء طفيف التوغل بسد الأوعية الدموية غير الطبيعية التي تُغذي الالتهاب دون التأثير على الأنسجة السليمة. تُظهر الدراسات السريرية نسبة نجاح تصل إلى 79.8٪ مع استمرار تقليل الألم لأكثر من عامين بعد الإجراء. بفضل ملف السلامة الإيجابي الذي يتمتع به والقدرة على تأخير جراحة استبدال المفصل، يُقدم AE الأمل في الحفاظ على نمط حياة نشط مع الحفاظ على مفصلك الطبيعي. تعرف على كيفية قيام هذا العلاج بالأشعة التداخلية المبتكر بتغيير مشهد إدارة التهاب المفصل التنكسي وتوسيع الخيارات للمرضى الذين يبحثون عن بدائل للأساليب التقليدية.
التحدي المتزايد لالتهاب المفصل التنكسي: أزمة صحية عالمية
يمثل التهاب المفاصل الكبيرة – مفصل الكتف، ومفصل الكوع، ومفصل الركبة، ومفصل الورك، ومفصل الكاحل – أكثر من مجرد تشخيص طبي. بالنسبة للمرضى، فهذا يعني الألم المستمر، ومحدودية الحركة، وعدم القدرة على الحفاظ على النشاط البدني المنتظم، وتدهور كبير في جودة الحياة.
عبء التهاب المفصل التنكسي يمتد إلى ما هو أبعد من المعاناة الفردية. مع تأثر الملايين في جميع أنحاء العالم، فإن التأثير الاقتصادي من خلال تكاليف الرعاية الصحية وفقدان الإنتاجية يكون كبير. تشمل عوامل الخطر العمر، والسمنة، وإصابات المفاصل، والاستعداد الوراثي، والضغوط الوظيفية التي تفرض ضغطاً متكرراً على المفاصل.
لسوء الحظ، فإن الداء المفصلي التنكسي (التهاب المفصل التنكسي) لا يمكن شفاؤه. باعتبارنا فريقاً طبياً مخصصاً لإيجاد حلول مبتكرة، فإننا نشعر بالقلق بشكلٍ خاص إزاء الاتجاه المثير للقلق المتمثل في تشخيص الاعتلال المفصلي في أعمار أصغر سناً، خاصةً بين الرياضيين والأفراد النشطين بدنياً.
كما تُظهر الأبحاث، فإن تنكس مفصل الركبة يظل الشكل الأكثر انتشاراً، حيث يؤثر على حوالي 13٪ من النساء و 10٪ من الرجال الذين تتراوح أعمارهم بين 60 عاماً فما فوق. ومع ذلك، فإننا نشهد زيادات مثيرة للقلق في جميع أشكال تنكس المفصل، مما يجعل البحث عن تدخلات فعالة أكثر أهمية من أي وقت مضى.
| المفصل المتأثر | الانتشار | المجموعات الأكثر تأثراً |
|---|---|---|
| الركبة (داء مفصل الركبة) | حوالي 13٪ من النساء و 10٪ من الرجال | أكثر شيوعاً لدى الذكور |
| الورك (فصال الورك) | حوالي 3-6٪ من البالغين | أكثر شيوعاً لدى الإناث |
| الكتف | حوالي 2-5٪ من البالغين | الرياضيون، والعمال اليدويون |
| الكوع | حوالي 1-3٪ من البالغين | الرياضيون (خاصة رياضات الرمي)، ومهن معينة |
| الكاحل | حوالي 1٪ من البالغين | الرياضيون السابقون، حالات ما بعد الصدمة |
* بيانات البروفيسور الدكتور في الطب أتيلا كوفاكس
مشهد العلاج الحالي وحدوده
النهج التقليدي لإدارة التهاب المفصل (الفصال العظمي) يتبع عادةً تقدماً تدريجياً من التدابير المحافظة إلى التدخلات الأكثر توغلاً مع تَقدُم المرض.
الإدارة الدوائية حالياً تتضمن ما يلي:
- الأدوية المضادة للالتهاب غير الستيرويدية NSAIDs لعلاج آلام التهاب المفصل وتقليل الالتهاب، متاحة كأدوية عن طريق الفم أو تطبيقات موضعية
- الكورتيكوستيرويدات (الستيرويد القشري) يتم إعطاؤها عن طريق الفم أو عن طريق حقن المفصل لتقليل الالتهاب
- الأدوية المضادة للروماتيزم المُعدلة للمرض والأدوية البيولوجية الأحدث لأنواع محددة من التهاب المفاصل الالتهابي
أساليب العلاج الطبيعي تركز على ما يلي:
- التمارين الرياضية لتحسين نطاق حركة المفاصل
- الجبائر أو الأقواس للدعم في الحالات المؤهلة
- العلاج الإشعاعي منخفض الجرعة المضاد للالتهابات
تدخلات التنظير المفصلي تتضمن تقنيات مثل:
- تقنيات تجديد الغضروف: الكسر الدقيق والكسر النانوي
- تكون الغضروف الذاتي المستحث بالمصفوفة - AMIC
- CartiFill - مصفوفة الكولاجين الغضروفية ثلاثية الأبعاد
- زرع الخلايا الغضروفية الذاتية (ACI)
- زرع الطُعم الذاتي العظمي الغضروفي (ОАТS)
على الرغم من أن تقنيات تنظير المفصل هذه تمثل تقدماً كبيراً، وخاصةً بالنسبة لتلف الغضروف الموضعي، إلا أنها تواجه قيوداً عند علاج تنكس المفصل الأكثر انتشاراً والذي يُعد نموذجياً في حالات التهاب المفصل المتوسطة إلى المتقدمة.
أوجه القصور في طرق الإدارة المحافظة
لسوء الحظ، فإن الأساليب التقليدية لها حدود واضحة. تُقدم الأدوية راحة مؤقتة فقط مع المخاطرة بحدوث آثار جانبية، ولا يمكن للعلاج الطبيعي استعادة الوظيفة، وحتى تقنيات تنظير المفصل المتطورة تساعد فقط في علاج الضرر الموضعي.
الحقيقة القاسية التي نلاحظها هي أنه جميع المرضى الذين يعانون من التهاب المفصل التَقدُمي تقريباً يحتاجون في نهاية المطاف إلى استبدال المفصل (الأطراف الاصطناعية الداخلية) عندما تفشل الإجراءات المحافظة. وهذا يخلق سيناريو مثير للقلق:
- تتمتع البدلة الاصطناعية الداخلية بعمر خدمة أقصى يبلغ حوالي 15 عاماً، وغالباً ما تتطلب الاستبدال بعد 10 سنوات فقط لدى الأفراد النشطين جسدياً
- عادةً ما يكون من الممكن تنفيذ إجراء أو إجراءين فقط لاستبدال مفصل واحد
- يؤدي هذا إلى خلق حالة حرجة للمرضى الأصغر سناً الذين قد يواجهون دمج المفصل (القَسَطُ) والتثبيت الدائم في سنواتهم الأخيرة إذا خضعوا للاستبدال في وقت مبكر جداً
هذا يؤكد الأهمية الحاسمة لتطوير التدخلات التي يمكن أن تؤجل بشكل فعال الحاجة إلى جراحة استبدال المفصل. يمثل كل عام مكتسب قبل إجراء تركيب المفاصل الاصطناعية الداخلية وقتاً ثميناً للحفاظ على وظيفة المفاصل الطبيعية والحفاظ على الخيارات المستقبلية.
المسار الالتهابي: هدف جديد للتدخل
لقد تطور فهم الداء المفصلي التنكسي بشكلٍ كبير خلال السنوات الأخيرة. وبعيداً عن كونه مجرد حالة "تآكل وتلف"، فإننا ندرك الآن أن التهاب المفصل هو اضطراب التهابي معقد حيث تلعب مكونات الأوعية الدموية دوراً حاسماً في تَقدُم المرض وظهور الأعراض.
في الداء المفصلي التنكسي، تنمو الأوعية الدموية غير الطبيعية من الشرايين المحيطة (مثل الشرايين الركبية في الركبة) إلى أنسجة المفصل والعظم. تُصبح هذه الأوعية ملتهبة أو مضغوطة أثناء حركة المفاصل، مما يُسبب الألم، والتورم، وتقييد وظيفي تَقدُمي.
لا يمكن المبالغة في أهمية هذا المسار الوعائي. يؤدي الالتهاب الزليلي (التهاب بطانة المفصل) إلى سلسلة من الوسائط الالتهابية، بما في ذلك البروتين المتفاعل-C، والبروستاجلاندين prostaglandins، والسيتوكينات، وعوامل النمو. تساهم هذه البيئة الالتهابية بشكل مباشر في انهيار الغضروف، وتضيق مساحة المفصل، وتَقدُم المرض.
يمثل الانصمام الشرياني (AE) إجراءً جديداً طفيف التوغل لعلاج الداء المفصلي التنكسي. من خلال استهداف المسار الالتهابي مباشرةً عند مصدره الوعائي، تعمل هذه التقنية على معالجة آلية أساسية لتقدُم المرض بدلاً من مجرد علاج الأعراض. بالنسبة للمرضى الذين يسعون إلى تأجيل أو تجنُب استبدال المفصل، يوفر AE بديلاً واعداً يحافظ على سلامة المفصل مع معالجة الألم والالتهاب.
ما يجعل الانصمام الشرياني ذو قيمة فريدة هو النهج المُستهدِف لهذه الآلية المُسببة للأمراض المحددة. بدلاً من قمع الالتهاب على نطاق واسع في جميع أنحاء الجسم (كما هو الحال مع الأدوية المضادة للالتهاب غير الستيرويدية NSAIDs) أو تقليل الالتهاب الموضعي مؤقتاً (كما هو الحال مع حقن الستيرويد)، فإن AE يقاطع بدقة إمداد الأوعية الدموية الذي يُغذي العملية الالتهابية.
وكما لاحظ فريق البحث لدينا، فإن هذا النهج يتماشى مع الفهم الحالي بأن الداء المفصلي التنكسي لا ينطوي فقط على التدهور الميكانيكي ولكن أيضاً على مكونات التهابية ووعائية نشطة يمكن تعديلها باستخدام التدخلات المُستهدِفة.
التدخلات الوعائية: تغيير نموذج العلاج
يمثل الانصمام الشرياني لالتهاب المفصل نهجاً ثورياً حقاً للحفاظ على المفصل. إن هذا الإجراء بسيط للغاية ولكنه متطور في استهداف آليات المرض.
أثناء التدخل، يقوم أخصائي الأشعة التداخلية بعمل ثقب صغير، عادةً في منطقة الفخذ، للوصول إلى النظام الشرياني. يتم توجيه قسطرة دقيقة إلى الشرايين المحددة التي تُغذي الغشاء الزليلي الملتهب في المفصل المتأثر باستخدام توجيه التصوير المتخصص. يتم بعد ذلك تسليم جزيئات صمية صغيرة بدقة لسد (إحصار) هذه الأوعية غير الطبيعية، مما يؤدي بشكل فعال إلى "تقليم" شبكة الأوعية الدموية التي تُغذي الالتهاب دون التأثير على تدفق الدم الطبيعي إلى الأنسجة السليمة.
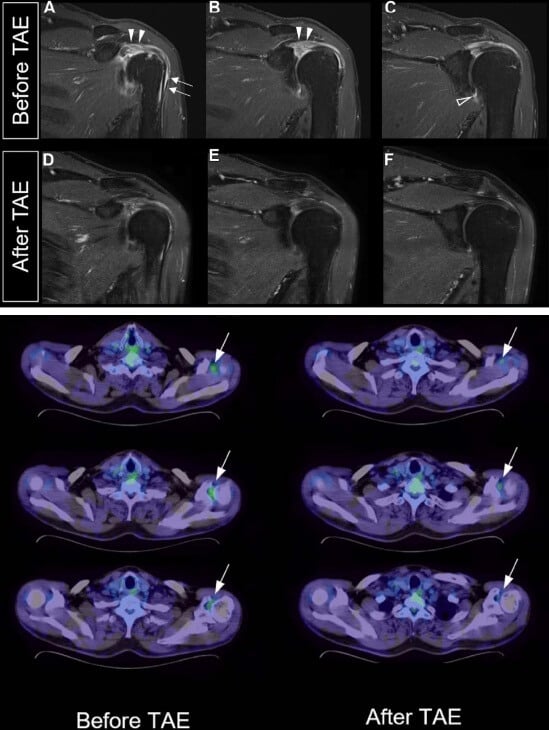
تسمح تقنيات التصوير المتقدم للمفصل، بما في ذلك تصوير المفصل باستخدام التباين (تصوير المفصل بالرنين المغناطيسي)، بتصور دقيق لشبكات الأوعية الدموية غير الطبيعية المستهدفة عن طريق الانصمام، مما يعزز الدقة التشخيصية وتخطيط العلاج.
يستغرق الإجراء بأكمله عادةً حوالي ساعة واحدة لإكماله، ويخرج المرضى في نفس اليوم. يتم إجراء تقييم المتابعة في غضون شهر لتقييم تَحسُن الأعراض ومراقبة أي مضاعفات محتملة.
في حين أن المبادئ العامة تظل مُتسقة، فإن التقنية تتطلب تهييئات محددة للمفاصل المختلفة:
- الركبة (انصمام الشريان الركبي / GAE): يستهدف الشرايين الركبية المحيطة بمفصل الركبة، مع اهتمام تجنيبي بالفروع الشريانية التي تُغذي الجلد والأنسجة المحيطة. يُقدم هذا النهج أفضل علاج لـ الداء المفصلي التنكسي في مفصل الركبة وعلاج مفصل الركبة الفعال بدون جراحة.
- الكتف (انصمام شريان الكتف / SAE): يركز على فروع الشرايين فوق الكتف، وتحت الكتف، والشرايين المنعطفة التي تُغذي الالتهاب الزليلي، مما يتطلب تنقلاً دقيقاً لتجنب الهياكل الوعائية الحرجة في هذا المفصل المعقد. يوفر هذا الإجراء علاجاً فعالاً لالتهاب مفصل الكتف وعلاج آلام مفصل الكتف للمرضى الذين يبحثون عن الراحة.
- الكوع (انصمام شريان الكوع / EAE): يعالج الشرايين الجانبية الكعبرية والزندية المتكررة، مع إيلاء اهتمام خاص لشبكة الأعصاب الكثيفة في هذه المنطقة. يمثل هذا التدخل علاجاً مبتكراً لالتهاب المفصل في الكوع، ويستهدف المسارات الوعائية المحددة التي تساهم في آلام التهاب مفصل الكوع.
- الورك (انصمام شريان الورك / HAE): يستهدف الفروع المفصلية للشرايين الفخذية والشرايين السدادية، مما يوفر خيار علاج جديد لفصال مفصل الورك مع نتائج واعدة. أصبح هذا النهج معترف به باعتباره أفضل علاج للداء المفصلي التنكسي في الورك بين الخيارات طفيفة التوغل.
- الكاحل (انصمام شريان الكاحل / AAE): يركز على فروع الشرايين الظنبوبية الأمامية والخلفية، مما يوفر علاجاً جديداً لألم مفصل الكاحل يعالج المكون الوعائي للالتهاب في هذا المفصل الحامل للوزن.
كفريق طبي ملتزم بتطوير رعاية المرضى، يجب علينا التأكيد على أن تقنية الانصمام الوعائي للداء المفصلي التنكسي لا تزال غير متاحة على نطاق واسع نظراً لندرة المتخصصين ذوي الخبرة في هذه التقنية. هذا يمثل تحدياً كبيراً في المجال – وهو نقص الأطباء المتخصصين فيما نعتقد أنه يمثل مستقبل علاج الداء المفصلي التنكسي.
من هو المُرشح الجيد لـ AE؟
يوفر الانصمام الشرياني خيار علاج قيم لمجموعة واسعة من المرضى المصابين بالداء المفصلي التنكسي. بناءً على خبرتنا السريرية ونتائج الأبحاث، يشترك المرشحون المثاليون عادةً في عدة خصائص:
- الأفراد النشطون الذين يسعون إلى الحفاظ على قدرتهم على الحركة وجودة حياتهم
- البالغون الذين تبلغ أعمارهم 35 عاماً فأكثر والذين يعانون من الداء المفصلي التنكسي
- أولئك الذين يعانون من آلام المفصل المتوسطة إلى الشديدة على الرغم من التدابير المحافظة
- الأفراد الذين لم يتعرضوا لتحسُن يذكر مع العلاجات التقليدية، مثل العلاج الستيرويدي الموجه بالموجات فوق الصوتية أو أدوية الألم
- المرضى الذين ليسوا مرشحين بعد لاستبدال المفصل أو يرغبون في تأجيل هذا الخيار
تُعتبر هذه التقنية ذات قيمة خاصة للمرضى الذين يواجهون قرارات علاج صعبة، بما في ذلك:
- أولئك الذين ليسوا مستعدين نفسياً لإجراء جراحة استبدال المفاصل الكبرى
- المرضى الذين يُعتبرون مرشحين ضعفاء لإجراء الجراحة بسبب الأمراض المصاحبة مثل داء السكري أو السمنة
- المرضى الأصغر سناً الذين قد يؤدي تأخير استبدال المفصل لديهم إلى منع جراحات المراجعة المتعددة في وقت لاحق من حياتهم
- الأفراد المصابون بالتهاب المفاصل العظمي "الرطب" الذي يتميز بالالتهاب الزليلي النشط والانصباب المفصلي، والذين يستجيبون بشكلٍ جيد لهذا النهج الذي يستهدف الأوعية الدموية
يقوم المتخصصون السريريون لدينا، الذين يركزون على حلول التهاب المفصل المبتكرة، بتقييم حالة كل مريض بعناية لتحديد ما إذا كان الانصمام الشرياني يمثل تدخلاً مناسباً في رحلة إدارة الداء المفصلي التنكسي.

الأدلة السريرية ونتائج المرضى
تستمر الأدلة السريرية الداعمة للانصمام الشرياني في علاج الداء المفصلي التنكسي في النمو، حيث أظهرت دراسات متعددة نتائج مُشجعة عبر العديد من مقاييس النتائج الرئيسية.
أظهرت دراسة استطلاعية أُجريت على 72 مريضاً (95 ركبة، بما في ذلك المرضى الذين لديهم مؤشرات لاستبدال مفصل الركبة) المصابين بالداء المفصلي التنكسي من الدرجة 1-3 وفقاً لمقياس Kellgren-Lawrence، معدل نجاح سريري بلغ 79.8٪ (95٪ CI و ٪69-٪87) بعد ثلاث سنوات من إجراء انصمام الشريان الركبي genicular artery embolization. الأهم من ذلك أن متابعة التصوير بالرنين المغناطيسي لتشخيص المفصل بعد عامين أظهرت تحسناً كبيراً في الالتهاب الزليلي مقارنةً بخط الأساس (p = 0.0016) دون وجود دليل على تنخر العظم أو تَقدُم التغيرات التنكسية.
ملفات الأمان لهذا العلاج الذي يُعدّ حالياً أفضل علاج لالتهاب مفصل الركبة، أظهرت نتائج إيجابية بشكل ملحوظ، حيث كانت الأحداث الضارة بسيطة وعابرة في الغالب. الأثر الجانبي الأكثر شيوعاً الذي تم الإبلاغ به هو تغير لون الجلد المؤقت في موقع العلاج، والذي يختفي عادةً دون تدخل.
بيانات تخفيف الألم على المدى القصير والطويل
من الجدير بالملاحظة بشكلٍ خاص التحسُن التقدُمي في درجات الألم بمرور الوقت، مما يقترح أن فوائد الانصمام قد تستمر في التطور بعد فترة ما بعد العملية مباشرةً. يُشير البحث إلى أن الانصمام الشرياني فعال ودائم في تقليل أعراض الألم الناجمة عن الداء المفصلي التنكسي المعتدل أو الشديد الذي أثبت مقاومته للعلاجات المحافظة الأخرى، كل ذلك مع الحفاظ على ملف أمان مقبول.
| النقطة الزمنية | متوسط درجة الألم* | نسبة الانخفاض من خط الأساس** |
|---|---|---|
| خط الأساس | 12.1 | – |
| شهر | 6.2 | ٪48.8 |
| 4 أشهر | 4.4 | ٪63.6 |
| 6 أشهر | 3.7 | ٪69.4 |
| 12 شهراً | 3.0 | ٪75.2 |
| 24 شهراً | 2.6 | ٪78.5 |
*استناداً إلى درجة مؤشر الألم المرتبطة بالداء المفصلي التنكسي في جامعات أونتاريو الغربية وماكماستر
** بيانات البروفيسور الدكتور في الطب أتيلا كوفاكس.
التحسينات الوظيفية عبر المفاصل المختلفة
بالإضافة إلى الحد من ألم الداء المفصلي التنكسي، تم توثيق تحسينات وظيفية عبر أنواع متعددة من المفاصل بعد الانصمام الشرياني:
علاج التهاب مفصل الركبة:
- تحسينات كبيرة في مسافة المشي والقدرة على صعود الدرج
- تقليل التيبس الصباحي وتحسين القدرة على القيام بالأنشطة اليومية
- تعزيز المشاركة في الأنشطة الترفيهية ذات التأثير المنخفض
علاج التهاب مفصل الكتف:
- في دراسة أُجريت على 15 مريضاً يعانون من الكتف المتجمد تم علاجهم بالانصمام، لوحظت ارتباطات كبيرة بين انخفاض امتصاص FDG (مقياس الالتهاب) وتحسينات في كلا من درجات مقياس الألم (p = 0.039) والقدرة على التمديد (p = 0.026)
- تحسين نطاق الحركة، خاصةً في الدوران الخارجي والإبعاد
- تعزيز القدرة على أداء الأنشطة العامة وتقليل الألم الليلي
- يوفر علاج الالتهاب الزليلي في مفصل الكتف تحسناً شاملاً في وظيفة المفصل
علاج التهاب مفصل الكوع:
- انخفاض ملحوظ في الالتهاب الزليلي كما أظهرت دراسات التصوير
- تحسين قوة قبضة اليد والاستخدام الوظيفي للذراع
- انخفاض الألم أثناء الراحة والنشاط
إدارة التهاب مفصل الورك:
- أظهر العلاج الجديد للداء المفصلي التنكسي في مفصل الورك تحسينات كبيرة في الراحة لتحمل الوزن ومسافة المشي
- تقليل متطلبات مسكنات الألم وتحسين جودة النوم
علاج التهاب مفصل الكاحل:
- يُظهر العلاج الجديد لألم مفصل الكاحل من خلال الانصمام نتائج واعدة بشكلٍ خاص في حالات ما بعد الصدمة
- تحسين الاستقرار والراحة أثناء المشي والوقوف
- انخفاض الألم والتورم مع النشاط
هذه التحسينات الوظيفية تُترجم إلى تحسينات ذات معنى في جودة الحياة، مما يسمح للعديد من المرضى باستئناف الأنشطة التي كانوا قد تركوها سابقاً بسبب ألم المفصل والقيود.
تَجنُب أو تأخير جراحة استبدال المفصل
أحد أهم الفوائد المحتملة للانصمام الشرياني هي التأجيل أو التَجنُب المحتمل لجراحة استبدال المفصل. تُظهر دراسات المتابعة لدينا للمرضى الذين خضعوا لهذه الإجراءات ما يلي:
- العديد من المرضى الذين كانوا يُعتبرون في السابق مُرشحين لاستبدال المفصل الوشيك تمكنوا من تأخير الجراحة لسنوات بعد الانصمام
- الحفاظ على وظيفة المفصل الأصلية يتجنب القيود المتأصلة في المفاصل الاصطناعية
- يمثل كل عام من التأجيل الحفاظ على خيارات العلاج المستقبلية، وهو أمر ذو قيمة خاصة للمرضى الأصغر سناً الذين قد يواجهون جراحات مراجعة متعددة
- طبيعة الانصمام طفيفة التوغل لا "تحرق الجسور" - فلا يزال بإمكان المرضى متابعة علاجات أخرى، بما في ذلك استبدال المفصل في نهاية المطاف إذا لزم الأمر، دون أي تنازلات
كفريق طبي ملتزم بالرعاية التي تركز على المريض، فإننا نرى أن هذه القدرة على الحفاظ على وظيفة المفصل الطبيعية وتوسيع الجدول الزمني لـ البدلة الاصطناعية الداخلية لمفصل الورك، والبدلة الاصطناعية الداخلية لمفصل الركبة، والبدلة الاصطناعية الداخلية للكوع، باعتبارها ربما الجانب الأكثر قيمة في تقنيات الانصمام الشرياني.
مقارنة الفعالية: التقليدية مقابل الجديدة
تُسلط هذه المقارنة الضوء على الموقع الفريد للانصمام الشرياني في طيف العلاج، مما يوفر تخفيفاً كبيراً للألم وتحسيناً وظيفياً مع إمكانية تعديل المرض، كل ذلك من خلال العلاج طفيف التوغل مع نتائج دائمة والحد الأدنى من المضاعفات.
دراسات انصمام الشريان الركبي مقابل الاجتثاث تُظهر باستمرار أن الانصمام يوفر راحة طويلة الأمد مع آثار جانبية أقل، مما يجعله أفضل طريقة لعلاج التهاب المفاصل المستمر والألم. يعتبر العديد من المتخصصين أن الانصمام الشرياني هو أفضل شيء حدث في رعاية المفاصل التداخلية في السنوات الأخيرة.
| نهج العلاج | تخفيف الألم | التحسُن الوظيفي | الغزوية | مدة التأثير | المضاعفات |
|---|---|---|---|---|---|
| NSAIDs / المسكنات | مُعتدل | الحد الأدنى | لا توجد | ساعات إلى أيام | مخاطر الجهاز الهضمي، والقلب، والكلى مع الاستخدام طويل الأمد |
| حقن الستيرويد القشري (العلاج الموجه بالموجات فوق الصوتية، العلاج بالحقن الموجه بالتصوير المقطعي المحوسب) | جيد (قصير الأمد) | مُعتدل (قصير الأمد) | منخفضة | 1 - 3 أشهر | احتمال تلف الغضروف مع الاستخدام المتكرر |
| العلاج الطبيعي | خفيف إلى متوسط | مُعتدل | لا توجد | متغيرة | الحد الأدنى |
| إجراءات التنظير المفصلي | مُعتدل | مُعتدل | مُعتدلة | 1 - 2 سنوات | مخاطر جراحية، ونتائج متغيرة |
| الانصمام الشرياني | ممتاز | جيد | منخفضة | تم توثيقها لأكثر من عامين، ومن المحتمل أن تكون أطول | الحد الأدنى، وعادةً ما تكون عابرة |
| استبدال المفصل | ممتاز | جيد | مرتفعة | 10 - 15 سنة أو أقل | مخاطر جراحية، وقيود المراجعة |
الوصول إلى الرعاية المبتكرة مع Booking Health
محدودية توافر العلاجات المبتكرة مثل الانصمام الشرياني يخلق حواجز كبيرة أمام المرضى الباحثين عن بدائل لاستبدال المفصل. في Booking Health، وضعنا على عاتقنا مهمة سد هذه الفجوة من خلال ربط المرضى بالخبرة المتخصصة اللازمة لهذه التدخلات المتطورة، وتبسيط الوصول إلى الرعاية الطبية الدولية.
نحن نُقدم الدعم الشامل للمرضى الذين يسعون للحصول على علاجات مبتكرة لالتهاب المفصل من خلال نهج شخصي يتضمن:
- تقييم الخبراء لحالتك والاتصال بالمرافق المتخصصة مع المتخصصين التداخليين ذوي الخبرة
- تطوير برامج علاجية فردية في مراكز معترف بها دولياً دون فرض أقساط على المرضى الأجانب
- التنسيق الطبي واللوجستي الكامل، بما في ذلك التوثيق، والمواعيد، والتغطية التأمينية
- دعم السفر مع خدمات النقل، والإقامة، والمترجم الفوري عند الحاجة
- إدارة الرعاية المستمرة، بما في ذلك شراء الأدوية والتواصل مع المتخصصين بعد العلاج
التزامنا الأساسي هو صحتك وضمان حصولك على أفضل دواء والرعاية الأكثر تقدماً لحالتك. من خلال تسهيل الوصول إلى التدخلات المتخصصة مثل الانصمام الشرياني، نأمل في توسيع إمكانيات العلاج الخاصة بك ودعم رحلتك العلاجية نحو صحة المفاصل وجودة حياة أأفضل.
لكل مريض قصة: رحلات Booking Health العلاجية المُلهمة
الأسئلة الشائعة لمرضانا
أرسل طلب للعلاجيختلف العلاج الأمثل باختلاف الفرد، لكن الانصمام الشرياني يوفر علاجاً بديلاً واعداً للداء المفصلي التنكسي الذي يستهدف الالتهاب في مصدره الوعائي مع الحفاظ على سلامة المفاصل.
تستخدم تقنيات التدخل الإشعاعي radiological intervention مثل الانصمام الشرياني التوجيه التصويري لاستهداف آليات المرض بدقة، ومعالجة الالتهاب الوعائي الأساسي بدلاً من مجرد إخفاء الأعراض كما تفعل العديد من العلاجات التقليدية.
توفر التدخلات الموجهة بالصور (أي الحقن) تخفيف مؤقت للألم يستمر لمدة تتراوح من شهر إلى ثلاثة أشهر، في حين تُظهر التدخلات الأحدث لعلاج الالتهاب الزليلي في المفصل انخفاضاً في الألم يستمر لأكثر من عامين بعد الإجراء.
يُعد انصمام شريان الكتف (SAE) أفضل علاج لألم التهاب مفصل الكتف، حيث يستهدف الشرايين التي تُغذي الالتهاب الزليلي مع تحسينات كبيرة في درجات الألم ونطاق الحركة.
يمثل انصمام الشريان الركبي علاجاً جديداً لفصال مفصل الركبة بنسبة نجاح سريرية موثقة تبلغ 79.8٪ خلال ثلاث سنوات، ومن المحتمل أن يكون بمثابة بديل لاستبدال مفصل الركبة.
علاج التهاب مفصل الركبة بدون جراحة ممكن من خلال التدخلات الوعائية الدموية مثل إجراء انصمام الشريان الركبي، والذي يعمل على سد (إحصار) الأوعية الدموية غير الطبيعية التي تُغذي الالتهاب مع الحفاظ على ملف أمان مناسب.
تشمل الفوائد الحد بشكلٍ كبير من الألم والتأجيل المحتمل لخطر استبدال المفصل، في حين أن المخاطر تكون في الغالب طفيفة وعابرة، وتقتصر عادةً على تغير لون الجلد المؤقت في موقع العلاج.
بَرز انصمام الشريان الركبي كأفضل علاج لألم مفصل الركبة، حيث أظهرت الدراسات تَحسُن تَقدُمي مع مرور الوقت من خلال معالجة مسارات الأوعية الدموية الالتهابية بشكلٍ مباشر من خلال علاج الالتهاب الزليلي في مفصل الركبة.
تقنية GAE هي علاج غير جراحي طفيف التوغل لألم مفصل الركبة، يستخدم جزيئات صمية صغيرة لسد (إحصار) الأوعية الدموية غير الطبيعية التي تُغذي التهاب المفصل، مما يؤدي بشكل فعال إلى (تقليم) شبكة الأوعية الدموية التي تدعم العملية الالتهابية.
تُظهر الدراسات السريرية نسبة نجاح تصل إلى 79.8٪ بعد ثلاث سنوات من العلاج، مع تَحسُن كبير في الالتهاب الزليلي وتقليل الألم بشكل تَقدُمي، مما يجعله علاجاً بديلاً رائداً لـ الداء المفصلي التنكسي في مفصل الركبة.
يتضمن التدخل الإشعاعي radiological intervention عادةً الخروج من المستشفى في نفس اليوم مع الحد الأدنى من وقت التعافي، مع توفير تخفيف جيد للألم دون المساس بخيارات العلاج المستقبلية.
اختر العلاج في الخارج وستحصل بالتأكيد على أفضل النتائج!
المؤلفون:
تم تحرير المقال من قبل خبراء طبيين وأطباء معتمدين من مجلس الأطباء الدكتورة ناديجدا إيفانيسوفا و الدكتور فاديم جيلوك. لعلاج الحالات المشار إليها في المقال، يجب استشارة الطبيب؛ المعلومات الواردة في المقالة ليست مخصصة للتطبيب الذاتي!
سياستنا التحريرية، التي توضح بالتفصيل التزامنا بالدقة والشفافية، متاحة هنا. انقر على هذا الرابط لمراجعة سياساتنا.
المصادر:
The University of Chicago Medical Center
Journal of Vascular and Interventional Radiology (JVIR)
اقرأ:
قائمة المقالات:
لا تعرف من أين تبدأ؟
اتصل بـ Booking Health